Functional medicine focuses on identifying and addressing the root causes of diseases. Functional medicine doctors employ a systems-oriented approach, often working with patients over an extended period to address the genetic, biochemical, and lifestyle factors that influence complex, chronic diseases. They are typically board-certified in their primary specialty and then receive additional training in functional medicine.
Doctors in functional medicine can be MDs (Medical Doctors) or DOs (Doctors of Osteopathic Medicine). Both MDs and DOs complete accredited medical schools and residency programs; however, MDs follow an allopathic approach focused on diagnosing and treating diseases, while DOs also incorporate osteopathic manipulative medicine, which emphasizes a holistic approach and the body’s musculoskeletal system in health and disease. After their formal medical training, doctors can pursue further education in functional medicine from various institutions, such as the Institute for Functional Medicine or universities offering certifications in Human Nutrition and Functional Medicine.
While not all functional medicine practitioners are MDs, many are. The rise of functional medicine has seen an increasing number of MDs expand their expertise to include its practices and philosophies, aligning with a more patient-centered approach to health care. This integration allows them to bridge the gap between conventional and alternative medicine, providing comprehensive care to their patients.

I am a Nurse Practitioner licensed across multiple states, with experience in cardiology, nephrology, and family medicine. My current focus is on primary care, where I advocate for a holistic approach to healthcare, often recommending functional medicine to patients when suitable.
Definition of Functional Medicine
Functional medicine is an individualized, patient-centered, science-based approach that empowers patients and practitioners to work together to address the underlying causes of disease and promote optimal wellness. This approach hinges on a detailed understanding of each patient’s genetic, biochemical, and lifestyle factors and leverages that data to direct personalized treatment plans.
Key Features:
- Holistic: Considers the body as an interconnected whole
- Patient-Centric: Treats the patient, not just the symptoms
- Evidence-Based: Relies on the latest research to guide treatment
Functional medicine involves a deep dive into a patient’s history and biochemistry to develop a comprehensive picture of health. This includes but is not limited to:
- Detailed medical histories
- Genetic data
- Lifestyle choices and behaviors
Practitioners of functional medicine may include medical doctors (MDs), osteopathic doctors (DOs), naturopathic doctors (NDs), and other credentialed healthcare professionals who have undergone additional training in functional medicine.
Functional medicine aims to provide strategies for:
- Prevention: Through diet, nutrition, and exercise
- Management: Using integrative therapies
- Reversal: Addressing lifestyle changes and environmental exposures
Its patient-specific treatment plans may incorporate a combination of traditional Western medical practices with integrative medicine and therapies. It is not unusual for functional medicine treatments to involve aspects of nutrition, detoxification, stress reduction, and exercise.
Educational Path of Functional Medicine Doctors
Functional medicine doctors often start with the same rigorous medical education as MDs before specializing in their field. They must meet specific education and training requirements, including attending an accredited medical school, completing a residency program, and obtaining certification.
Medical School Accreditation
To become a functional medicine doctor, one must first graduate from an accredited medical school. Medical schools that qualify typically hold accreditation from organizations such as the Liaison Committee on Medical Education (LCME) in the United States. Graduates obtain a Doctor of Medicine (MD) degree. Some may also obtain a Doctor of Osteopathic Medicine (DO) degree, which emphasizes a whole-person approach to treatment.
Residency and Training
After medical school, a prospective functional medicine doctor must complete a residency in a chosen specialty. This can be in areas like family medicine or internal medicine, which provide a broad foundation for holistic patient care. During residency, they receive extensive clinical training under supervised conditions, gaining experience in diagnosing and managing a variety of health conditions.
Certification Process
Upon completing residency, physicians can pursue additional training in functional medicine. Certification in functional medicine is available through institutions that specialize in this area, such as the Institute for Functional Medicine. The certification process often includes the completion of several courses, passing examinations, and demonstrating clinical experience in functional medicine practices. This certification underscores a physician’s expertise and dedication to the principles of functional medicine, which can include nutrition, lifestyle modifications, and other integrative approaches.
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
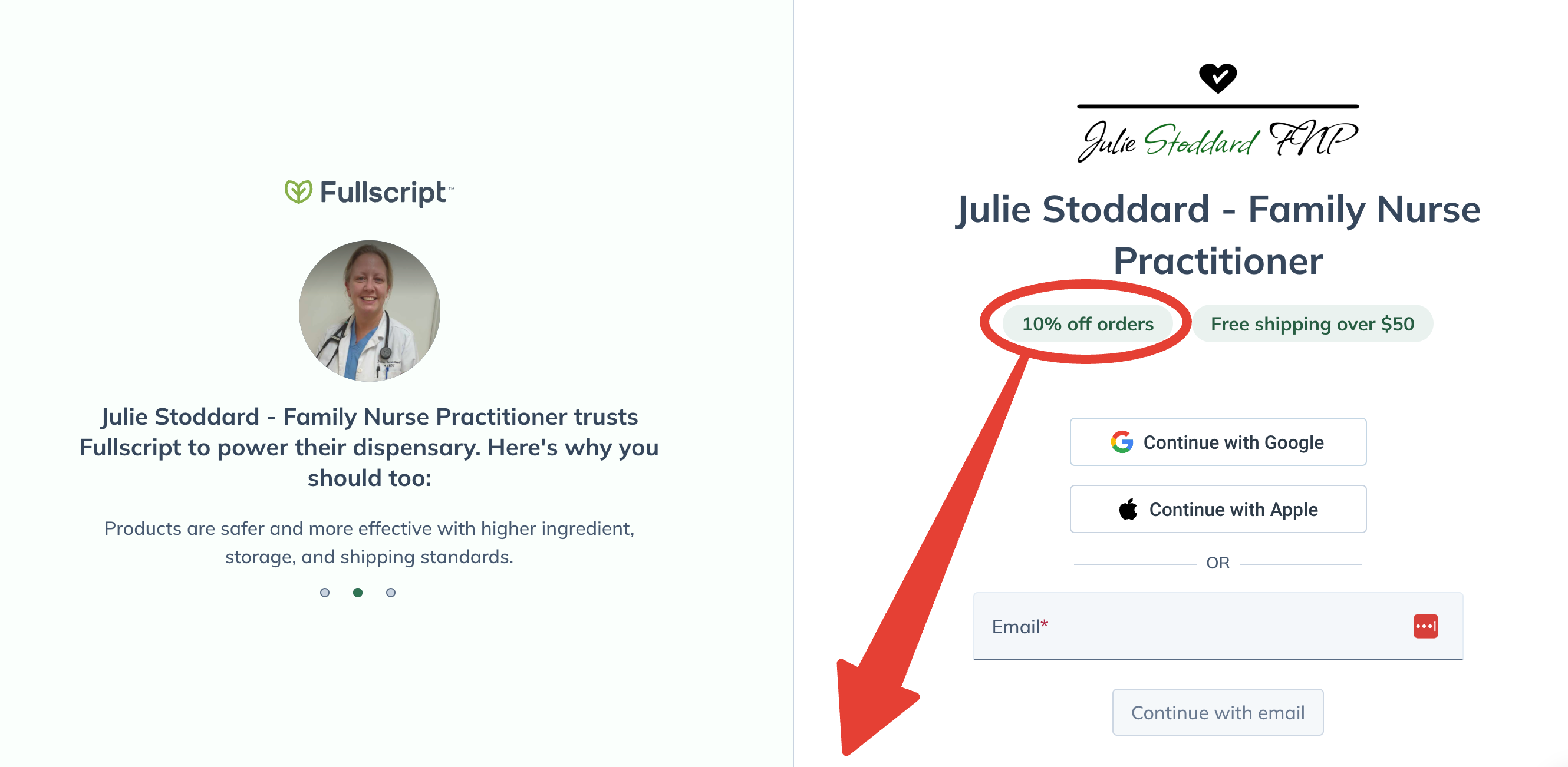
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
MDs Versus DOs in Functional Medicine
Functional medicine often integrates traditional medical practices with a more holistic approach to patient care. Both MDs (Doctor of Medicine) and DOs (Doctor of Osteopathic Medicine) can specialize in functional medicine, but they come from distinct philosophical backgrounds and training paths.
Differences in Philosophies
MDs (Allopathic Physicians): Traditionally, MDs focus on the diagnosis and treatment of diseases using conventional methods. In functional medicine, MDs apply these principles but also incorporate a systems-oriented approach, looking at the complex web of interactions in the patient’s history, physiology, and lifestyle that can lead to illness.
DOs (Osteopathic Physicians): DOs are trained to take a more holistic view of medical care from the beginning, emphasizing preventive health care and the body’s musculoskeletal system. In functional medicine, DOs naturally align with the practice’s principles, focusing on the whole person rather than isolated symptoms.
Training and Practice
MDs: MDs undergo a traditional medical education and may later receive training in functional medicine through fellowships, continuing education, or certification programs from institutions like the Institute for Functional Medicine. Their approach in functional medicine is evidence-based and rooted in modern scientific research.
DOs: All DOs are trained in osteopathic manipulative treatment (OMT), a hands-on approach to help diagnose and treat illnesses and injuries. When practicing functional medicine, DOs combine their unique training with functional medicine’s systems biology approach, often focusing on prevention and lifestyle factors.
Both MDs and DOs must be licensed to practice medicine and can choose to pursue additional certification in functional medicine to deepen their expertise in this area.
Functional Medicine Certification for MDs
Physicians often pursue functional medicine certification to enhance their ability to provide patient-centered care and to apply an integrative approach to treatment. This certification typically involves rigorous education and evaluation processes specifically designed for MDs and DOs.
Eligibility Requirements
According to the Institute for Functional Medicine (IFM), the eligibility requirements for their Functional Medicine Certification Program (IFMCP) in the United States include holding at least a master’s level degree in a health-related field from an accredited university. Additionally, applicants must hold an active healthcare license to practice by the appropriate authority in their state, province, or country.
Curriculum and Examination
The curriculum for functional medicine certification generally comprises multiple areas of study, including but not restricted to:
- Systems biology
- Biochemical individuality
- Patient-centered care
- Lifestyle factors
These are taught in various modules that cover in-depth topics in nutrition, genetics, and the latest research on environmental and lifestyle impacts on health.
After completing the required coursework, physicians must pass a comprehensive examination that tests their knowledge and ability to apply functional medicine in clinical scenarios. This exam is a critical component of the certification process and is designed to maintain high standards of practice within the field.
Approaches and Modalities in Functional Medicine
Functional medicine is distinguished by its focus on personalized care and comprehensive treatment strategies. This approach holistically considers each patient’s unique genetic, biochemical, and lifestyle factors.
Personalized Treatment Plans
Functional medicine practitioners develop personalized treatment plans that cater to the individual’s medical history, genetics, and health goals. The aim is to not just relieve symptoms but also address root causes of illness. For instance, if a patient presents with chronic digestive issues, the practitioner may assess diet, stress levels, and a range of environmental factors before creating a targeted plan that could include dietary changes, supplements, and stress-reduction techniques.
Integrative Techniques
In functional medicine, integrative techniques are employed in unison with conventional medicine practices. These may involve nutritional therapy, exercise recommendations, or mind-body interventions such as meditation. Practitioners often utilize advanced laboratory testing to gather detailed information about a patient’s health, which informs the integrative techniques applied for treatment. For example, genetic testing might reveal predispositions to certain conditions, guiding the practitioner in tailoring a diet that manages those risks.
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
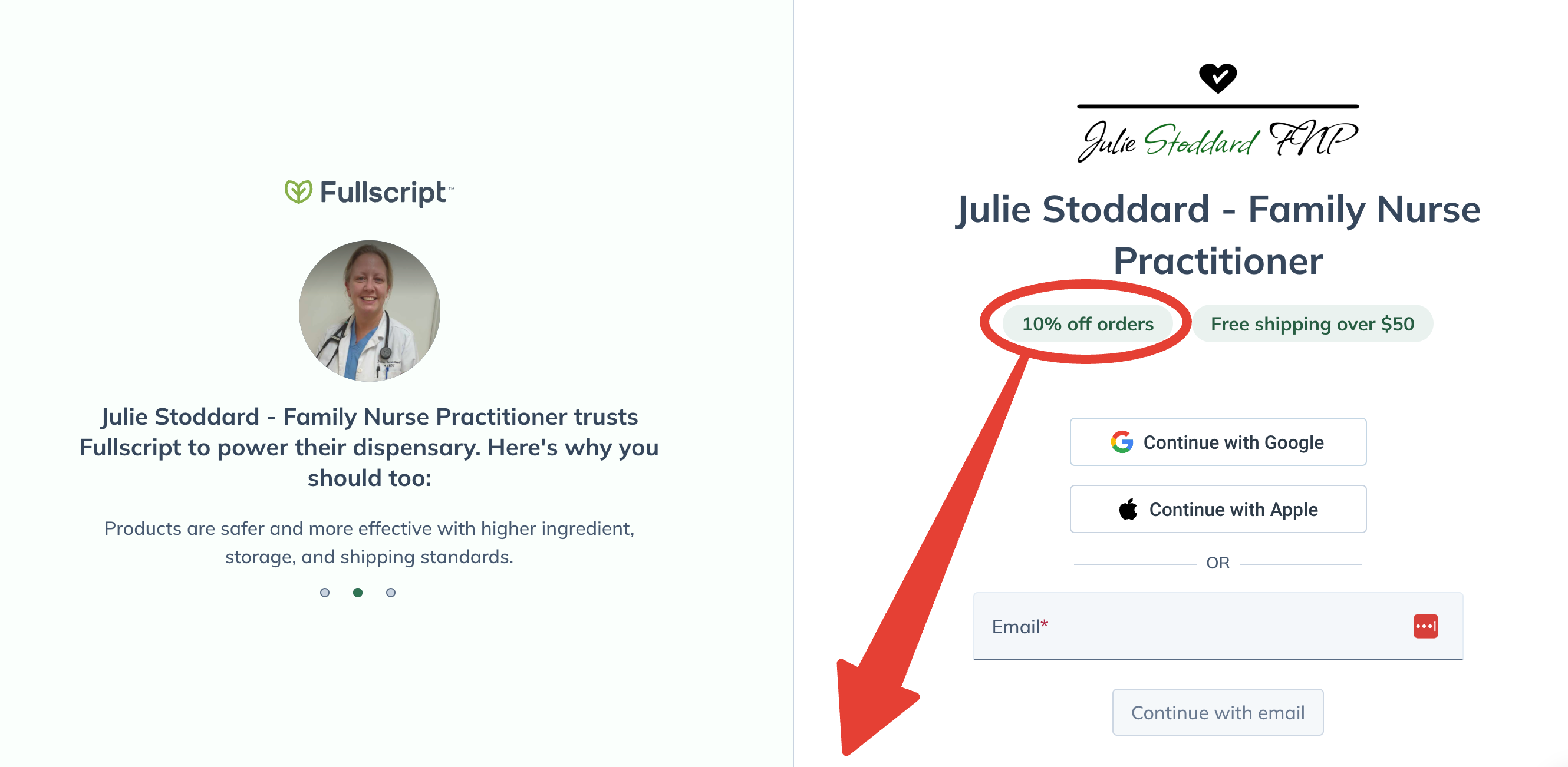
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
The Role of Functional Medicine Doctors
Functional medicine doctors focus on personalized healthcare, tailoring treatment to the individual patient, often in the context of chronic disease management and preventive care.
Chronic Disease Management
In managing chronic diseases, functional medicine doctors adopt a systems-oriented approach, seeking to identify and treat the underlying causes of a condition rather than merely addressing symptomatic relief. They typically spend extensive time with their patients, examining not only medical history but also lifestyle choices that may influence long-term health outcomes.
Preventative Health Care
Prevention is a cornerstone of functional medicine, with practitioners emphasizing the importance of nutrition, exercise, and stress management as key components. They work with patients to develop comprehensive wellness plans that promote sustainable health behaviors and proactively reduce the risk of disease development.
Research and Evidence in Functional Medicine
Functional medicine emphasizes individualized, patient-centered care and often integrates traditional medical practices with alternative treatments. When it comes to the basis of functional medicine, a strong foundation in peer-reviewed research is crucial to validate its approaches. The field assesses various biological systems to understand disease causality, striving to address root causes rather than just symptoms.
In educational settings, such as the program offered by University of Western States, curricula integrate evidence-based research to keep pace with evolving scientific understanding. This evidence is critical in reinforcing functional medicine’s legitimacy and effectiveness.
Clinical research underscores functional medicine by focusing on areas like:
- Genetic predisposition
- Environmental factors
- Lifestyle influences on health
Programs, like the ones provided by John Patrick University, prepare healthcare professionals to use these research lenses in practice. They learn to evaluate how multiple factors contribute to wellness or disease, supporting treatments that are both integrative and tailored to the individual.
Current research integrates concepts such as nutrition, epidemiology, and disease prevention — all imperative in the functional medicine model. For example, studies may investigate how dietary changes can modify gene expression relevant to health outcomes, an approach in line with principles touted by institutions like Saybrook University, which delves into holistic nutrition.
While functional medicine is still growing and evolving, the incorporation of rigorous research supports an evidence-based approach, crucial for the continued acceptance and validation within the wider medical community.
Patient Experiences with Functional Medicine MDs
Functional Medicine MDs apply a systems-oriented approach and engage both patient and practitioner in a therapeutic partnership. It’s a shift from traditional disease-centered focus of medical practice to a more patient-centered approach.
Testimonials and Outcomes
Testimonials from patients often highlight personalized treatment plans and the MDs’ emphasis on understanding the patient’s genetic, biochemical, and lifestyle factors. Some patients have noted significant improvements in chronic conditions that were not adequately managed by conventional treatments. In particular, the holistic approach to gut health highlighted by Saybrook University emphasizes the impact of diet on genes and health, leading to positive patient outcomes.
- Chronic Illness Management: Patients have reported better management of conditions such as autoimmune diseases and gastrointestinal disorders.
- Improved Wellness: A focus on preventive health measures and nutritional education has empowered patients to make substantive lifestyle changes.
Critiques and Controversies
Despite positive reports, there have been critiques about functional medicine. Critics have pointed out a lack of large-scale studies and standardized protocols, leading to questions about the evidence-based nature of the practice. For example, a Harvard study on healthcare practices revealed significant variations in care between physicians, underscoring the need for consistent application of evidence-based guidelines.
- Variability in Treatment: Divergent approaches among Functional Medicine MDs may lead to inconsistent patient experiences.
- Cost and Accessibility: Concerns have been raised about the high out-of-pocket costs for treatments that might not be covered by insurance.
Regulation and Standards in Functional Medicine
Functional medicine emphasizes a more patient-centered approach than traditional allopathic medicine — focusing on the root causes of diseases. It employs a systems-oriented medical strategy that works across disciplines and is informed by evidence-based medicine. Practitioners may include MDs (Medical Doctors), DOs (Doctors of Osteopathic Medicine), NDs (Naturopathic Doctors), and more.
Regulatory bodies ensure that practitioners meet and maintain professional standards for practice. For instance, in the United States:
- Medical doctors (MDs) and doctors of osteopathic medicine (DOs) are licensed by state medical boards.
- Naturopathic doctors are regulated in states where Naturopathy is licensed.
The Institute for Functional Medicine (IFM), a leading education provider, sets standards for functional medicine training and certification. To become certified, practitioners must complete the IFM Certification Program.
Furthering the industry’s commitment to high standards, organizations such as the American Board of Physician Specialties (ABPS) offer board certification in integrative medicine. Certifications serve to indicate a practitioner’s commitment to ongoing education and competence in functional medicine.
Each certification demands rigorous training, exams, and commitment to patient care. As the field evolves, regulatory measures and standard-setting organizations continue to safeguard both the integrity of the profession and the well-being of the patients.
The Future of Functional Medicine
Functional Medicine is poised for transformative growth, propelled by technological innovation and its potential for integration into broader healthcare systems.
Technological Advancements
Technological advancements are set to significantly enhance the field of Functional Medicine. Cutting-edge diagnostics and big data analytics will provide deeper insights into patient health, allowing for more personalized care plans. With the promise of advancements such as machine learning models predicting disease patterns, practitioners will have access to tools that not only interpret complex biochemical data but also suggest optimal intervention strategies. For example, wearable health monitoring devices will enable continuous tracking of vital signs, contributing to more dynamic and responsive treatment approaches.
Integration into Mainstream Medicine
The integration of Functional Medicine into mainstream healthcare is a developing trend that shows no signs of abating. One can expect to see Functional Medicine principles increasingly adopted by traditional medical institutions, emphasizing preventive medicine and tailored treatment. This change is partly driven by a growing body of evidence that supports the efficacy of Functional Medicine approaches, such as those discussed in the UWS Human Nutrition and Functional Medicine program, which place a strong emphasis on nutrition and lifestyle intervention. Furthermore, collaborations between Functional Medicine practitioners and conventional healthcare providers will likely become more common, as both systems seek to improve patient outcomes while managing costs.
Choosing a Functional Medicine Practitioner
When seeking a functional medicine practitioner, it is imperative that individuals carefully evaluate credentials and formulate targeted questions to ensure the doctor’s approach aligns with their health needs.
Evaluating Credentials and Expertise
Functional medicine is a science-based discipline that requires substantial training beyond traditional medical education. Prospective patients should verify that a practitioner has a recognized medical degree, such as a Doctor of Medicine (MD) or a Doctor of Osteopathic Medicine (DO). Additional certification in functional medicine from an accredited institution, like the Institute for Functional Medicine, denotes specialized expertise in this field. An interested patient can explore programs like the Master of Science in Human Nutrition and Functional Medicine offered by the University of Western States for more information on the training these practitioners undergo.
Key Credentials To Look For:
- MD or DO degree
- Board certification in a relevant specialty (e.g., family medicine, internal medicine)
- Certification in functional medicine
Training doesn’t stop at degrees; ongoing education is essential. Patients should seek out practitioners who demonstrate a commitment to staying current with the latest research and clinical practices in functional medicine.
Questions to Ask
Before committing to a functional medicine practitioner, patients should engage in a direct dialogue to assess compatibility and approach. Key questions can include:
- Scope of Practice: “Can you describe your approach to treating chronic health conditions?”
- Treatment Philosophy: “How do you integrate conventional medicine with functional medicine in your practice?”
- Success Stories: “Can you share patient outcomes or case studies that demonstrate the effectiveness of your treatment plans?”
By asking such questions, patients can discern the practitioner’s depth of knowledge and determine if their practice philosophy is congruent with the patient’s health objectives. It’s also a chance to gauge the practitioner’s communication style and willingness to collaborate on health care.
Frequently Asked Questions
Functional medicine offers a unique approach to healthcare, which often raises numerous questions regarding its practice. Here, common queries are addressed to provide clarity on the role and expertise of functional medicine doctors.
What credentials do functional medicine doctors typically hold?
Functional medicine doctors often hold a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree. They may also have additional training and certification in functional medicine through organizations such as the Institute for Functional Medicine (IFM).
Can functional medicine doctors prescribe medication?
Yes, functional medicine doctors who are MDs or DOs are licensed to prescribe medication as warranted by their patient’s individual health needs, following the same legal and ethical guidelines as conventional medical practitioners.
How does functional medicine differ from conventional medicine?
Functional medicine differs from conventional medicine in that it focuses on identifying and addressing the root causes of diseases. Functional medicine emphasizes a patient-centered approach rather than a disease-centered one, incorporating personalized treatments that may involve lifestyle and dietary changes.
Are the practices of functional medicine practitioners recognized by the medical community?
Functional medicine practices are gaining recognition in the medical community, especially among those advocating for a more patient-centered, personalized healthcare approach. However, opinions on functional medicine can vary widely among healthcare professionals.
Do insurance plans usually cover services provided by functional medicine doctors?
Coverage for functional medicine services can vary considerably by insurance plan. Some insurers cover certain functional medicine consultations and treatments, whereas others may not. Patients often need to check with their insurance providers regarding the specifics of their coverage.
What are the common criticisms or challenges associated with functional medicine?
The common criticisms of functional medicine pertain to its non-traditional methods and the lack of extensive scientific research supporting some of its practices. Critics often call for more rigorous, evidence-based studies to validate these alternative approaches to healthcare.

