After undergoing a hysterectomy, a woman’s body requires time to heal and adjust to the physiological changes that follow the surgical procedure. Recovery is a critical phase where the focus is on healing and regaining strength. However, the longer-term implications of the surgery mean that women may also need to consider adjusting their nutrient intake to support their health post-surgery.
There is evidence that suggests certain vitamins and minerals could play a significant role in supporting the body’s recovery after a hysterectomy. For instance, some supplements may help address the hormonal imbalances caused by the removal of the ovaries, which often leads to a sudden onset of menopausal symptoms. Ensuring adequate nutrient intake is essential for maintaining cardiovascular health, which can be adversely affected after hysterectomy, as well as bone density, which may be compromised due to a decrease in estrogen levels.
Careful selection of supplements can aid the recovery process, support overall well-being, and help mitigate some of the long-term health consequences of hysterectomy. It’s important for patients to discuss with their healthcare providers which supplements are most beneficial for their specific health needs and recovery plan post-hysterectomy.

I am a Nurse Practitioner licensed across multiple states, with experience in cardiology, nephrology, and family medicine. My current focus is on primary care, where I advocate for a holistic approach to healthcare, often recommending functional medicine to patients when suitable.
Understanding Hysterectomy
A hysterectomy is a surgical procedure to remove a woman’s uterus and potentially other reproductive organs depending on the specific condition and medical recommendation.
Types of Hysterectomy
Total Hysterectomy: Involves the removal of the entire uterus, including the cervix. This is the most comprehensive type of hysterectomy.
Partial Hysterectomy: Only the upper part of the uterus is removed, leaving the cervix in place.
Radical Hysterectomy: Performed primarily when cancer is present, this procedure includes the removal of the uterus, cervix, the tissue around the uterus, and the upper part of the vagina.
Hysterectomy with Bilateral Salpingo-Oophorectomy: Includes the removal of the uterus, cervix, both ovaries, and the fallopian tubes.
Reasons for Hysterectomy
Fibroids: Noncancerous growths in the uterus can cause pain and bleeding.
Cancer: If present in the uterus, cervix, or ovaries, a hysterectomy might be necessary.
Endometriosis: This condition wherein uterine tissue grows outside the uterus can lead to a hysterectomy when other treatments fail.
Uterine Prolapse: The uterus descends into the vagina, which can be corrected with a hysterectomy for severe cases.
Post-Hysterectomy Recovery
After undergoing a hysterectomy, a woman’s body requires time to heal and adapt. The recovery process is divided into two critical phases: immediate post-operative care and the long-term healing journey. Each phase demands specific attention to rest, pain management, and monitoring for signs of infection or complications.
Immediate Post-Operative Care
In the initial hours and days following a hysterectomy, patients must prioritize rest and adhere to professional healthcare guidance to ensure a smooth beginning to their recovery. Pain is typically managed with prescribed medications, which should be taken as directed to alleviate discomfort. It is imperative to monitor the incision site for signs of infection, such as redness, swelling, or discharge, as well as being vigilant for fever, which can signal infection.
- Rest: Allocate ample time for sleep and avoid strenuous activities.
- Pain Management: Utilize medications as instructed; report unmanageable pain to a healthcare provider.
- Incision Care: Keep the area clean and dry; follow instructions for dressing changes if provided.
- Monitoring for Complications: Observe for any signs of infection or abnormal discharge and report to a healthcare professional.
Long-Term Recovery Process
The path to full recovery extends beyond the initial post-operative period and can be influenced by factors such as individual health status and the extent of the surgery. It is important for patients to maintain a gradual return to regular activities, with an awareness that the body needs time to heal completely. The focus during this period is not only physical but also encompasses the patient’s overall quality of life.
- Gradual Return to Activities: Resume normal activity levels according to the body’s tolerance and under medical advice.
- Support System: Engage with a support network of friends, family, and healthcare professionals for both physical and emotional aid.
Embedding healthy lifestyle choices into the recovery process can optimize healing and enhance overall well-being post-hysterectomy. It’s important for patients to follow their healthcare provider’s recommendations carefully and to communicate any concerns during follow-up appointments.
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
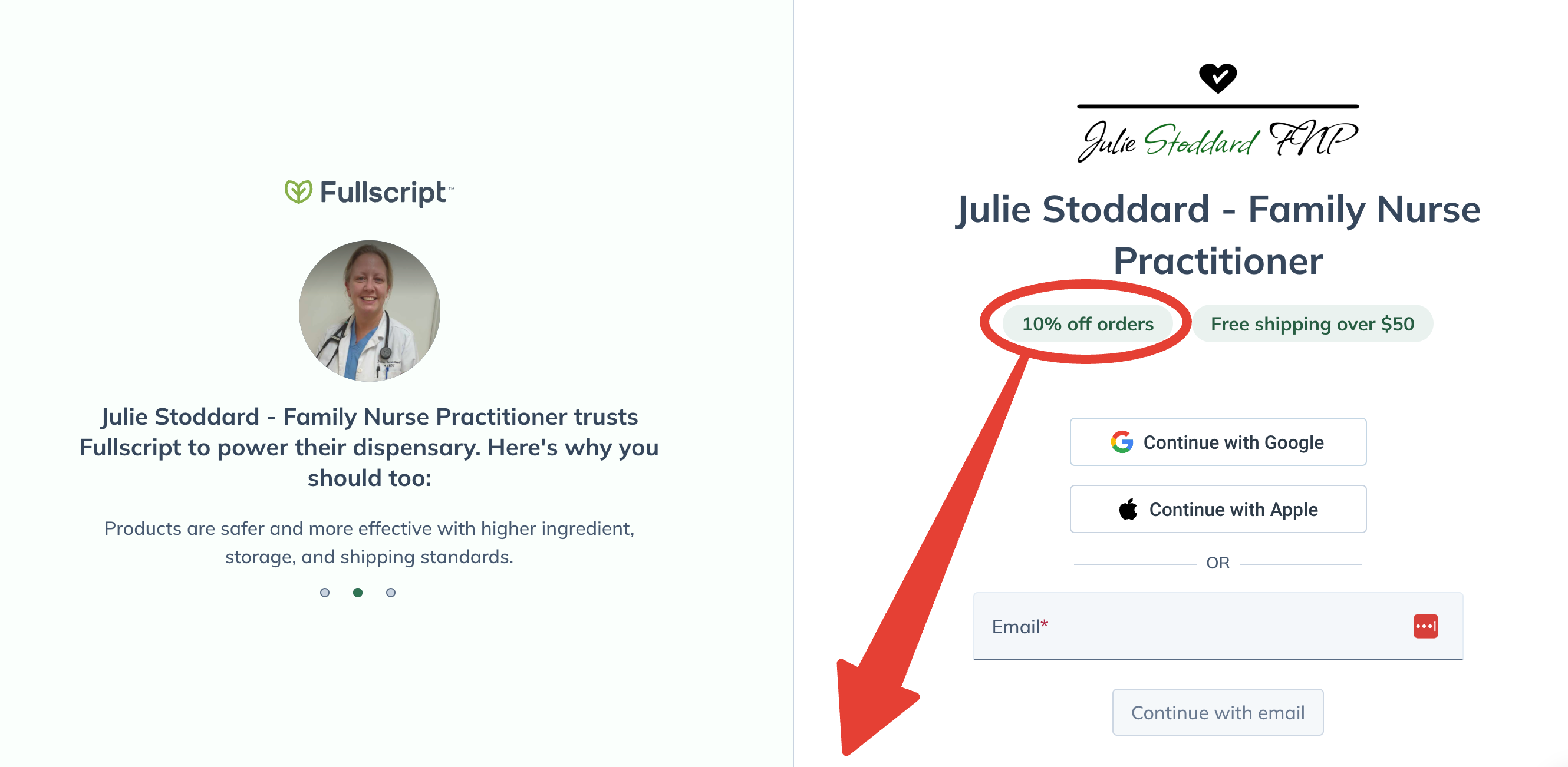
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
Physical Health Management
After a hysterectomy, it’s crucial to manage one’s physical health effectively to aid recovery and maintain overall wellness. Optimal nutrition and appropriate physical activity are key components of post-surgery care.
Exercise After Hysterectomy
Post-operative exercise: Initially, patients should focus on gentle activities like walking which can begin soon after surgery to promote circulation and prevent blood clots. As they recover, they can gradually include more strenuous exercises.
- Strength Training: Introducing light strength training to rebuild muscle is beneficial once the doctor approves. Aim for two to three times a week focusing on major muscle groups.
- Flexibility and Core Strengthening: Incorporating yoga or Pilates helps improve flexibility and strengthen the core, which can be especially helpful after abdominal surgeries like hysterectomy.
Weight Management Post-Surgery
Maintaining a healthy weight: Preventing weight gain is crucial as it can affect the recovery process and overall health.
- Balanced Diet: Ensuring a diet rich in lean proteins, whole grains, fruits, and vegetables supports muscle repair and can help manage weight effectively.
- Consistent Activity: Regular physical activity, as advised by a healthcare provider, is important to keep metabolism active.
Nutrition and Diet
After a hysterectomy, focusing on a nutrient-rich diet is essential for recovery and long-term health. Specific nutrients and food groups take on greater importance to assist in healing and maintaining hormonal balance.
Essential Nutrients
Post-hysterectomy, the body requires certain essential nutrients to aid in recovery and to compensate for the hormonal changes that occur. Calcium and vitamin D are critical for bone health, especially since the surgery can lead to an increased risk of osteoporosis. Including sources of omega-3 fats, which are anti-inflammatory, can help in healing and overall cell function. Protein, particularly lean protein, is vital for tissue repair and immune function. Foods rich in fiber promote digestive health and can help manage weight.
- Calcium: Aim for at least 1,200 mg/day through dairy products or fortified alternatives.
- Magnesium
- Vitamin D: 600 IU/day is recommended for most adults, which can be obtained through sun exposure and fortified foods.
- Omega-3 Fats: Include fish like salmon or take fish oil supplements as directed.
- Lean Protein: Incorporate chicken, turkey, fish, beans, and legumes into meals.
- Fiber: Aim for 25-30 g/day from vegetables, fruits, whole grains, and legumes.
Recommended Dietary Choices
A balanced diet consisting of a variety of fruits, vegetables, whole grains, and lean proteins can ensure that one is receiving a broad spectrum of nutrients necessary for recovery after a hysterectomy. Fruits and vegetables are rich in vitamins and antioxidants that support immune health and are an excellent source of fiber. Whole grains provide B vitamins and more fiber, which aids in maintaining a healthy gastrointestinal system and helps in feeling full, which can prevent overeating.
- Fruits: Berries, oranges, and apples are beneficial for their high vitamin and fiber content.
- Vegetables: Leafy greens, broccoli, and carrots are not only rich in fiber but also several key vitamins.
- Whole Grains: Oats, quinoa, and brown rice are good options for fiber and essential minerals.
- Lean Proteins: Legumes, tofu, and lean cuts of meat provide the necessary protein without excessive fat.
Incorporating these foods into a balanced diet can help one to not only recover post-operation but also to establish a healthy lifestyle moving forward.
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
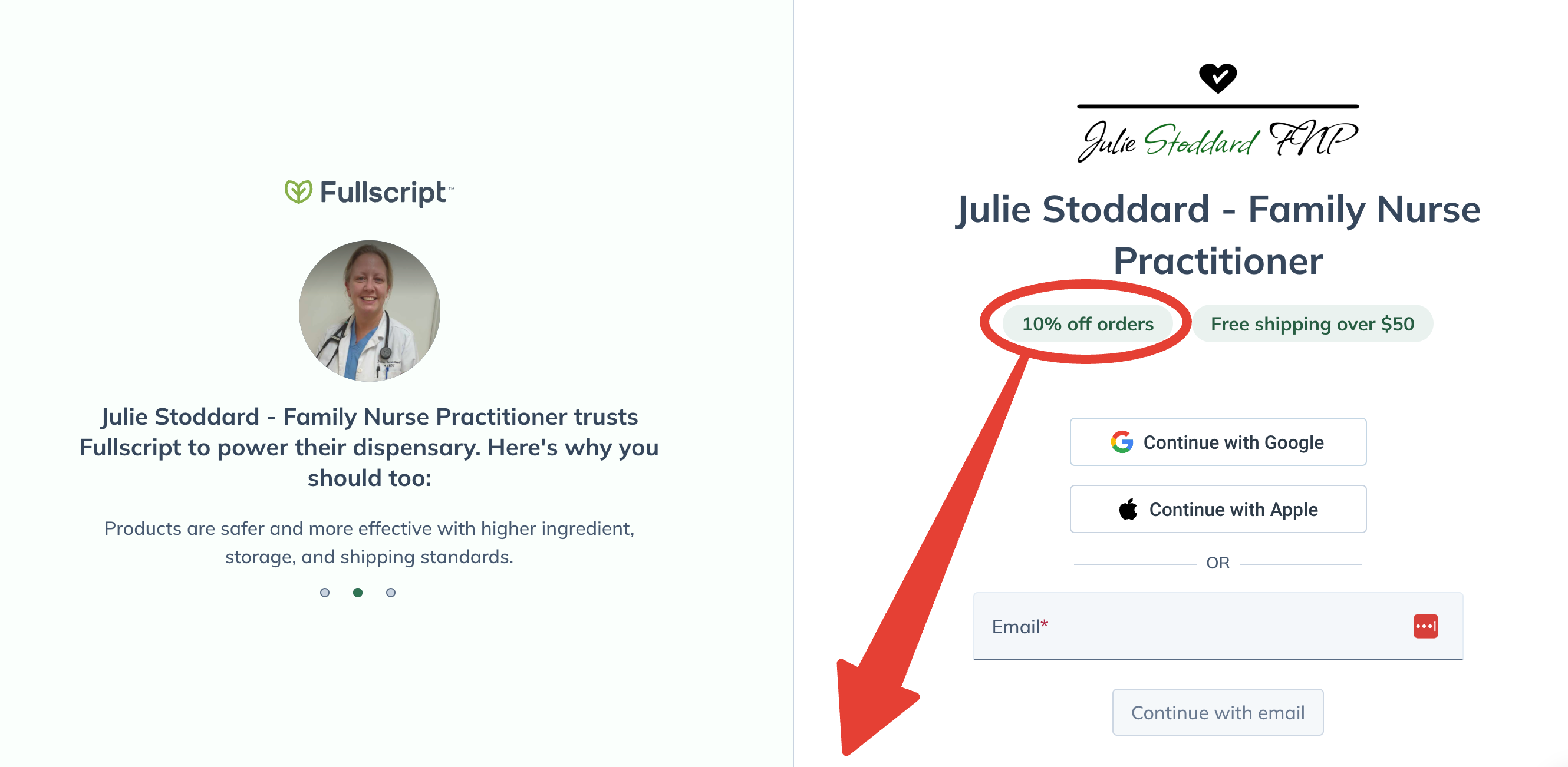
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
Supplementation Strategy
After a hysterectomy, a woman’s body may require additional support to recover and maintain balance. Precise supplementation can help mitigate the potential impacts on hormone levels, bone density, and overall wellness.
Key Supplements
Post-hysterectomy, key supplements address hormonal changes and nutrient needs. Estrogen levels often decline, making supplements like Vitamin D and magnesium essential for mood regulation. Omega-3 fatty acids are suggested for skin health and maintaining a positive mood.
Calcium and Bone Health
Calcium plays a crucial role in mitigating the risk of osteoporosis – a concern after hysterectomy due to potential impacts on bone density. A daily intake of calcium-rich supplements is recommended, paired with Vitamin D to enhance calcium absorption.
Vitamins for Overall Wellness
Vitamins are vital for overall wellness. A balanced multivitamin can replenish a woman’s nutritional profile post-surgery. B vitamins support energy levels and metabolism, whereas antioxidants like Vitamins C and E contribute to skin health and overall immune function.
Emotional and Mental Well-being
After a hysterectomy, women may experience significant emotional and mental health challenges due to hormonal changes and psychological implications. Addressing these challenges is critical for recovery and long-term well-being.
Coping With Hormonal Changes
Hormonal shifts can cause notable mood swings and irritability in women post-hysterectomy. Estrogen levels often decrease, leading to symptoms commonly associated with menopause. It is important to balance these hormonal fluctuations with appropriate supplements. For instance, phytoestrogen supplements, which contain estrogen-like substances found in some plants, could help balance hormones. Additionally, vitamin B complex supplements are known to aid in hormonal balance and mood regulation, aiding in the reduction of anxiety and stress.
Therapy and Support Networks
Engaging in therapy provides a structured approach to navigate emotional turbulence, such as depression or persistent feelings of sadness. Cognitive-behavioral therapy (CBT) has been beneficial for those experiencing mental health shifts after a hysterectomy, helping them address negative thought patterns. In addition, building a support network of friends and family is indispensable. Social support not only fosters feelings of joy and connection but also offers practical help during the recovery process. Group therapy or joining support groups specifically for women who have undergone hysterectomies can provide shared experiences and a sense of camaraderie, which can be especially comforting during this time.
Hormone Replacement Therapy
Hormone Replacement Therapy (HRT) is a treatment used to alleviate symptoms caused by the decrease in hormone levels following a hysterectomy. It primarily addresses issues such as hot flashes, night sweats, and vaginal dryness.
Understanding HRT
Hormone Replacement Therapy involves the administration of estrogen or a combination of estrogen and other hormones to remedy the deficits post-hysterectomy. There are different forms of HRT tailored to whether a woman has had a hysterectomy with or without bilateral oophorectomy. Women who have had their uterus removed typically receive estrogen-only therapy. However, if the ovaries are also removed, causing a more significant drop in hormone levels, they may need a combination of estrogen and other hormones like testosterone or progesterone.
Benefits and Risks
Benefits of HRT:
- Reduces menopausal symptoms: Effectively lessens the frequency of hot flashes and night sweats.
- Alleviates vaginal symptoms: Helps in treating vaginal dryness, thereby enhancing comfort and sexual health.
- May prevent bone loss: Estrogen has been noted to play a role in preserving bone density, potentially reducing the risk of osteoporosis.
Risks involved with HRT:
- Cardiovascular risks: There are concerns about an increase in the risk of heart disease, particularly for certain groups of women.
- Cancer risk: Specific formulations and durations of HRT may be associated with a higher risk of certain types of cancer.
- Other side effects: Some individuals may experience side effects such as bloating, breast swelling or tenderness, nausea, and headaches.
It is crucial for women to discuss the potential benefits and risks of HRT with their healthcare providers to make an informed decision tailored to their personal health situations.
Managing Menopause Symptoms
After a hysterectomy, managing menopause symptoms effectively becomes a primary concern for many women. This section provides targeted advice for a smoother natural menopause transition and for alleviating common symptoms, such as hot flashes, night sweats, and mood changes.
Natural Menopause Transition
For women experiencing natural menopause after a hysterectomy, the body undergoes a significant hormonal shift resulting in the cessation of menstrual periods. It’s important for them to focus on lifestyle adjustments and dietary considerations that support hormone balance. They should consume a diet rich in calcium and vitamin D or consider appropriate supplements to maintain bone density, which can be affected by menopause.
Alleviating Common Symptoms
- Hot Flashes: To reduce the frequency and severity of hot flashes, women may explore non-hormonal options, such as wearing layers for easy adjustment to changing body temperatures and avoiding triggers like spicy food, caffeine, and alcohol.
- Night Sweats: Ensuring a cool sleeping environment and possibly utilizing moisture-wicking bedding can provide relief from night sweats.
- Mood Changes: Regular physical activity, stress-reduction techniques, such as mindfulness or yoga, and support groups are beneficial for mood stability during this transition.
For symptomatic relief, there are medical interventions available, including hormone therapy, which should be considered based on individual symptoms and in consultation with a healthcare provider. Some women benefit from vasomotor symptoms management approaches that do not involve hormone treatments.
Sexual Health After Hysterectomy
After a hysterectomy, many women experience changes in their sexual health due to the removal of reproductive organs and potential hormonal adjustments. Understanding these changes and ways to enhance intimacy post-surgery is important for overall well-being.
Physiological Changes
The removal of the uterus—and occasionally the ovaries—can lead to hormonal fluctuations, primarily involving estrogen levels. Estrogen is crucial for maintaining the health and elasticity of vaginal tissues. Decreased estrogen may result in vaginal dryness, which can lead to discomfort during intercourse. To counteract this, women can consider estrogen therapy or personal lubricants that provide additional lubrication, thus maintaining sexual comfort.
Improving Intimacy
Intimacy after hysterectomy can be deeply affected by physical and psychological factors. Open communication with a partner about feelings and discomfort can foster a more understanding and supportive environment for sexual activity. For some women, sexual function improves after a hysterectomy, as per studies referenced in the narrative review by the National Center for Biotechnology Information, showing increased pleasure and orgasm frequency. Counseling and therapy may be beneficial in addressing emotional or psychological concerns, helping to improve sexual health post-hysterectomy.
Long-Term Health Risks
After a hysterectomy, attention to long-term health becomes crucial. Certain risks may escalate as the body adjusts post-surgery, particularly concerning bone and heart health.
Osteoporosis Risk
Post-hysterectomy, individuals may face an increased risk of osteoporosis due to a decrease in estrogen levels, especially if the ovaries are removed. Estrogen is vital for maintaining bone strength; its absence accelerates bone density loss, heightening the possibility of fractures. Intake of calcium and vitamin D supplements could be beneficial in mitigating this risk.
Heart Health
The removal of the uterus has been linked to a potential increase in the risk of heart disease and stroke, particularly when the ovaries are removed before natural menopause. Estrogen has a protective effect on the heart, and its sudden reduction can impact aging arteries. They may recommend regular cardiovascular exercise and a balanced diet rich in omega-3 fatty acids to support heart health.
Lifestyle Modifications
After a hysterectomy, a woman’s body undergoes significant changes, making lifestyle adjustments a crucial part of recovery. These changes can help manage symptoms and improve overall well-being.
Stress Reduction Techniques
Stress management is vital, as stress can exacerbate menopausal symptoms like hot flashes, which may follow a hysterectomy. Women can benefit from mindfulness meditation or yoga, both of which have been shown to reduce stress levels. Techniques like deep-breathing exercises or guided imagery can also be effective in promoting relaxation and rest. Incorporating these practices into one’s daily routine may aid significantly in the recovery process.
Creating a Balanced Life
Achieving balance in life involves ensuring adequate sleep, participating in activities that bring fun and joy, and making intentional lifestyle changes. Sleep hygiene practices, such as maintaining a consistent sleep schedule and creating a restful environment, are critical for healing. Additionally, one should prioritize rest throughout the day to conserve energy. Engaging in enjoyable activities can improve one’s mood and has positive effects on health. A balanced life following a hysterectomy should be a harmonious blend of rest, activities that provide a sense of fulfillment, and necessary lifestyle changes to support optimal health.

