Hyperparathyroidism is a condition characterized by the excessive production of parathyroid hormone (PTH) by the parathyroid glands located in the neck. This hormone plays a critical role in regulating calcium levels within the blood and bone metabolism. In normal function, these glands maintain calcium balance by releasing PTH when calcium levels are low. However, in hyperparathyroidism, one or more of the glands become overactive, leading to elevated levels of calcium in the blood, a condition known as hypercalcemia.
The most common form of this disorder is primary hyperparathyroidism, which typically arises from a benign growth on the parathyroid glands. Secondary hyperparathyroidism, another form of the ailment, occurs as a response to low calcium levels, often due to chronic kidney disease. This can cause the glands to become overworked and enlarged. Symptoms of hyperparathyroidism can be nonspecific and vary widely, ranging from bone and joint pain to weakness, fatigue, and in severe cases, kidney stones or osteoporosis.
Despite the array of potential symptoms, many patients with hyperparathyroidism are asymptomatic and are diagnosed during routine laboratory tests. The definitive management for the condition, especially when symptoms are present or complications arise, is surgical removal of the affected parathyroid tissue. Over the past few decades, surgical techniques have evolved, becoming more refined and resulting in higher success rates and fewer complications. Diagnosis and management strategies continue to improve, enabling more tailored approaches to treat this complex endocrine disorder.

I am a Nurse Practitioner licensed across multiple states, with experience in cardiology, nephrology, and family medicine. My current focus is on primary care, where I advocate for a holistic approach to healthcare, often recommending functional medicine to patients when suitable.
Fundamentals of Hyperparathyroidism
Hyperparathyroidism is a condition characterized by the overproduction of parathyroid hormone (PTH) by the parathyroid glands. These small glands are located behind the thyroid and regulate calcium levels in the body.
There are two primary types:
- Primary Hyperparathyroidism: This occurs when one or more of the parathyroid glands are overactive. The condition can lead to high levels of calcium in the blood, potentially causing a variety of symptoms and complications such as kidney stones, osteoporosis, and cardiovascular problems. Often, the only definitive management is a parathyroidectomy.
- Secondary Hyperparathyroidism: Often a result of other diseases like chronic renal failure, where reduced calcium absorption leads to compensatory overproduction of PTH.
Symptoms of hyperparathyroidism can include weakness, feeling tired, depression, joint pain, and fractures. The condition is diagnosed through blood tests that measure levels of calcium and PTH. High calcium levels and a raised level of PTH indicate hyperparathyroidism.
Treatments can vary depending on the cause and severity but may include surgical removal of the affected glands, medication to manage the symptoms, or observation in cases where symptoms are mild.
The adoption of routine chemistry panel testing in the 1970s has increased the discovery of primary hyperparathyroidism and changed its clinical presentation. The incidence of this disorder is estimated at around 66 per 100,000 person-years among women and 25 per 100,000 among men. Improved diagnostic strategies have also led to better management of primary hyperparathyroidism.
Etiology and Risk Factors
Hyperparathyroidism is characterized by the overproduction of parathyroid hormone (PTH) by the parathyroid glands. This condition primarily manifests in two forms: primary hyperparathyroidism (PHPT) and secondary hyperparathyroidism. Primary hyperparathyroidism is often caused by a benign tumor called an adenoma in one of the parathyroid glands. In rare instances, hyperparathyroidism can be due to parathyroid cancer.
The risk factors associated with primary hyperparathyroidism include:
- Gender and Age: Women over the age of 50 are at higher risk.
- Radiation: Previous radiation therapy targeted at the neck increases risk.
- Genetics: A family history of the disorder can predispose individuals.
Secondary hyperparathyroidism arises due to other conditions that cause low calcium levels in the body, prompting the parathyroid glands to increase PTH production. Risk factors for this form of hyperparathyroidism include:
- Vitamin D Deficiency: A deficient intake of vitamin D can lead to secondary hyperparathyroidism.
- Chronic Kidney Disease: Impaired kidney function may cause imbalances in calcium and phosphorus, triggering the disease.
To clarify the relationship between hyperparathyroidism and skeletal health, studies have shown that the condition may lead to site-specific reduction in bone mineral density, increasing the risk for fragility fractures.
Individuals with risk factors for hyperparathyroidism should undergo appropriate investigations, including measurements of serum calcium, to screen for the disorder. Regular monitoring and appropriate interventions can help manage this condition effectively.
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
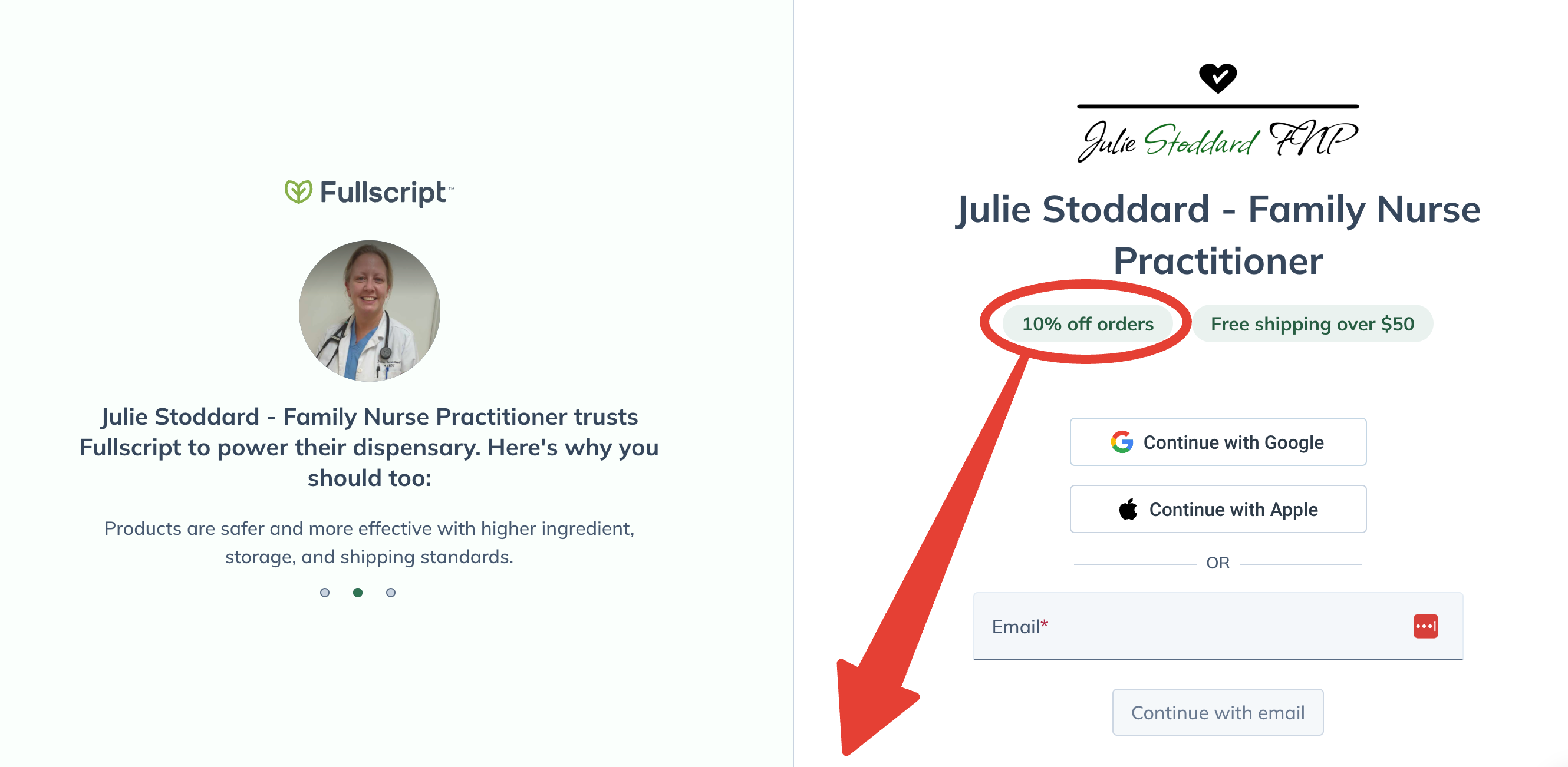
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
Types of Hyperparathyroidism
Hyperparathyroidism is categorized into three types: primary, secondary, and tertiary. Each type reflects a different underlying pathology affecting the parathyroid glands.
Primary Hyperparathyroidism
In primary hyperparathyroidism, one or more of the parathyroid glands produces excess parathyroid hormone (PTH). This condition is typically linked to a benign growth on a gland, known as a parathyroid adenoma. It can also result from hyperplasia of multiple glands or, rarely, parathyroid carcinoma. Elevated PTH leads to increased blood calcium levels, commonly resulting in bone loss, kidney stones, and neuromuscular symptoms.
Secondary Hyperparathyroidism
Secondary hyperparathyroidism arises not from the gland itself but as a response to low calcium levels often due to chronic kidney disease. The parathyroid glands are overstimulated to produce more PTH in an attempt to increase calcium levels, which can lead to bone disease and other systemic problems if prolonged.
Tertiary Hyperparathyroidism
Tertiary hyperparathyroidism is a progressive form of the condition that evolves from secondary hyperparathyroidism. It occurs when the parathyroid glands become unresponsive to the regulatory effects of serum calcium levels. This often happens after long-term secondary hyperparathyroidism, as seen in patients with end-stage renal disease who have undergone kidney transplantation.
Pathophysiology
Hyperparathyroidism is a condition characterized by the overactivity of one or more of the body’s parathyroid glands, which leads to the production of excessive amounts of parathyroid hormone (PTH). PTH is crucial for the regulation of serum calcium levels.
In primary hyperparathyroidism, the hypersecretion of PTH is typically due to a benign adenoma, hyperplasia, or rarely carcinoma of the parathyroid glands. This overproduction of PTH acts to increase the levels of calcium in the blood by:
- Increasing gastrointestinal calcium absorption through its effect on vitamin D metabolism
- Increasing renal calcium reabsorption, reducing the loss of calcium in urine
- Mobilizing calcium from the bone, thereby increasing bone resorption
Secondary hyperparathyroidism, on the other hand, is generally a consequence of chronic kidney disease, which leads to hypocalcemia and stimulates the parathyroid glands to produce more PTH in an attempt to maintain normal calcium levels.
- Decreased renal function in chronic kidney disease leads to phosphate retention, reduced vitamin D activation, and hypocalcemia.
A hallmark of hyperparathyroidism’s pathophysiology includes changes in bone mineral density, and patients may be predisposed to fragility fractures. A Dual-energy x-ray absorptiometry (DXA) examination is thus appropriate for those with hyperparathyroidism to screen for skeletal manifestations.
Symptoms and complications can be diverse due to the ubiquitous role of calcium in the body. However, it is crucial to recognize that hyperparathyroidism’s effects extend beyond hypercalcemia, potentially impacting cardiovascular health, kidney function, and even psychiatric well-being.
Signs and Symptoms
Hyperparathyroidism is characterized by an excess production of parathyroid hormone (PTH) from the parathyroid glands. This condition can lead to various signs and symptoms, primarily due to elevated calcium levels in the blood.
Common symptoms of hyperparathyroidism include:
- Fatigue: A pervasive sense of tiredness or weakness.
- Bone Pain and Fractures: Due to the demineralization of bones.
- Kidney Stones: Resulting from increased calcium levels in the urine.
- Abdominal Pain: Gastrointestinal discomfort can occur.
- Depression or Mood Changes: Neurological effects of high calcium levels may include altered mental status.
Patients may also experience:
- Muscle weakness
- Nausea or vomiting
- Increased thirst and frequent urination
Some individuals with hyperparathyroidism may be asymptomatic. They might only become aware of the condition upon the discovery of:
- Elevated calcium levels during a routine blood test
- A dual-energy x-ray absorptiometry (DXA) screening indicating reduced bone mineral density
The clinical presentation of hyperparathyroidism has shifted over time, with many cases now identified through routine screening rather than the severe symptoms seen in the past. Diagnosis often involves confirming high levels of PTH in the blood, particularly when high calcium levels are detected.
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
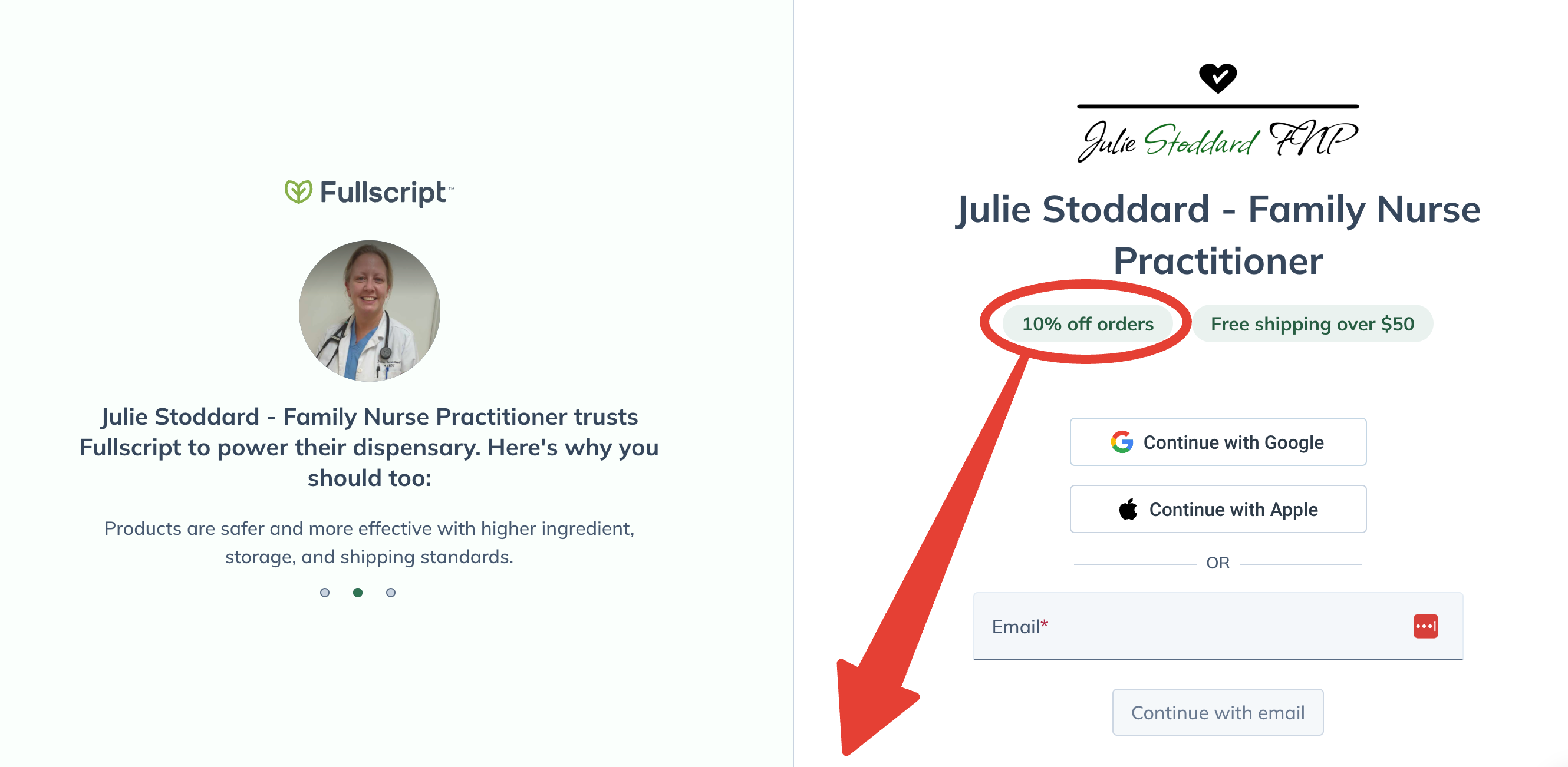
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
Diagnostic Evaluation
The diagnostic evaluation of hyperparathyroidism is a multi-step process aimed at confirming elevated parathyroid hormone levels and identifying the cause. Precise diagnosis typically involves blood tests, various imaging techniques, and differentiating the condition from other disorders with similar symptoms.
Blood Tests
Blood tests form the cornerstone of hyperparathyroidism diagnosis. These tests measure the levels of:
- Calcium: Elevated calcium levels may suggest hyperparathyroidism.
- Parathyroid Hormone (PTH): High PTH levels in conjunction with high calcium levels typically confirm the diagnosis.
These primary markers may be supplemented by checking levels of phosphorus, which are often low in hyperparathyroidism, and Vitamin D, which can influence calcium levels.
Imaging Techniques
If blood work indicates hyperparathyroidism, imaging tests help localize any abnormal parathyroid glands. Common imaging techniques include:
- Ultrasound: This non-invasive test can detect enlarged parathyroid glands.
- Sestamibi Scan: A more specific scan that uses a radioactive substance to pinpoint overactive parathyroid tissue.
These imaging tests are essential for preoperative planning, especially if surgery is being considered.
Differential Diagnoses
It’s crucial to differentiate primary hyperparathyroidism from other conditions that can cause similar symptoms, such as:
- Familial Hypocalciuric Hypercalcemia (FHH): A genetic condition that presents with high calcium levels, but normal to slightly elevated PTH levels.
- Secondary Hyperparathyroidism: Typically due to chronic kidney disease, vitamin D deficiency, or calcium malabsorption, where PTH levels are elevated in response to low calcium levels.
Physicians must eliminate these and other conditions to confirm the diagnosis of primary hyperparathyroidism and proceed with the most appropriate treatment.
Treatment Strategies
Effective management of hyperparathyroidism involves a balance between surgical and pharmacological therapies, with ongoing patient monitoring to ensure the best outcomes.
Surgical Interventions
Surgical removal of the affected parathyroid gland(s), known as parathyroidectomy, is considered the definitive treatment for primary hyperparathyroidism. According to guidelines published by the American Association of Endocrine Surgeons (AAES), this procedure is indicated when there is symptomatic disease, osteoporosis, kidney stones, or when calcium levels exceed certain thresholds. Minimally invasive techniques have improved the success rate and reduced recovery times.
Pharmacological Therapies
For patients who are not suitable candidates for surgery, medication can help control symptoms and manage the metabolic effects of the disease. Agents such as bisphosphonates, which help increase bone density, and calcimimetics, which can lower serum calcium levels, are commonly prescribed. Research highlighted in JAMA Internal Medicine points towards the significance of medication for patients who defer surgery or have persistent disease postoperatively.
Monitoring and Follow-up
Regular follow-up appointments are crucial to monitor the patient’s calcium levels and assess for any potential complications. Bone mineral density testing using dual-energy X-ray absorptiometry (DXA) scans is suggested for all patients with primary hyperparathyroidism, as per JAMA Surgery. These measures help in preventing complications and in adjusting treatment plans according to the patient’s evolving condition.
Complications and Prognosis
Hyperparathyroidism, specifically primary hyperparathyroidism (PHPT), can lead to a variety of health complications. The disorder is characterized by the overproduction of parathyroid hormone (PTH), which causes an imbalance in calcium levels. These imbalances impact multiple systems within the body.
Complications
Bone Health: Prolonged exposure to high PTH levels can result in a decrease in bone mineral density (BMD). This can make patients more susceptible to fragility fractures. It is recommended that patients undergo a Dual-energy x-ray absorptiometry (DXA) examination to screen for skeletal manifestations.
Renal Issues: If unabated, PHPT might lead to kidney stones or nephrocalcinosis due to elevated levels of calcium in the blood and urine.
Neuromuscular Symptoms: Patients might experience muscle weakness, fatigue, and in some cases, neuropsychiatric disturbances including depression and cognitive dysfunction.
Prognosis
With early detection and proper treatment, the prognosis for hyperparathyroidism is generally favorable. Surgical intervention, known as parathyroidectomy, is the common treatment approach and can lead to a significant improvement in symptoms and complications. Despite the associated risks, like voice changes due to nerve damage or short-term postoperative hypocalcemia, surgery often results in an increase in bone density and a decrease in the risk of fractures.
It is imperative for patients to be monitored regularly after treatment. Delays in diagnosis or treatment can exacerbate complications and negatively impact patients’ quality of life, as evidenced by increased disease sequelae in patients whose workup or time from diagnosis to treatment exceeded one year according to research published in JAMA Network Open. Therefore, timely medical intervention is critical in managing health outcomes for those with hyperparathyroidism.
Patient Management and Education
Management and education of patients with primary hyperparathyroidism (PHPT) is a critical aspect of care. Physicians often recommend routine monitoring of calcium levels, and patients may be advised to stay well-hydrated and engage in regular weight-bearing exercises to support bone health.
Dietary Considerations Patients should be educated about dietary choices, emphasizing a balanced intake of calcium-rich foods without overt supplementation unless instructed by a healthcare provider.
Medication Management If medication is prescribed, such as bisphosphonates, patients should receive clear instructions about dosing and any potential side effects. Compliance with medication regimes is crucial for managing symptoms and preventing complications.
| Activity | Purpose |
|---|---|
| Routine blood tests | To monitor calcium and parathyroid hormone levels |
| Regular consultations | To adjust treatment plans as necessary |
| Bone density scans | To assess bone mineral density |
Education extends to the potential need for surgery, which can be a curative treatment. Detailed education about the procedure and recovery can alleviate patient anxiety and clear any misconceptions. The importance of post-operative care should be emphasized to ensure optimal recovery and maintenance of calcium levels.
When educating patients, materials should be easy to understand and healthcare professionals should be open to answering questions, ensuring patients are well-informed of their condition and all potential management strategies.
Current Research and Developments
Recent studies in the realm of hyperparathyroidism have shed light on various aspects of disease progression and management. An investigation highlighted the consequences of delayed diagnosis and treatment of primary hyperparathyroidism (PHP), indicating that prolonged times to diagnosis can lead to increased disease sequelae.
Researchers are also focusing on the epidemiology and changing clinical presentations of the disease. An overview of PHPT demonstrated evolved clinical characteristics due to the advent of routine chemistry panel testing, drastically changing its diagnosis and management.
Moreover, expert panels have been working on developing comprehensive guidelines for managing primary hyperparathyroidism, involving a multi-disciplinary approach that encompasses endocrinologists, pathologists, surgeons, and radiologists.
The impact of parathyroidectomy on comorbidities and clinical outcomes in patients is another focus area. Research has suggested that untreated patients face a significantly higher risk of hip fractures, general fractures, and cardiovascular events, whereas those undergoing parathyroidectomy possibly exhibit lower risks.
These developments represent a significant stride towards understanding and improving patient outcomes in hyperparathyroidism through scientific inquiry and medical advancement.
Frequently Asked Questions
In this section, readers will find answers to common questions about hyperparathyroidism, including its signs, causes, types, and the importance of managing calcium levels to prevent complications.
What are the most common signs and symptoms of hyperparathyroidism?
The most typical manifestations of hyperparathyroidism include weakened bones, kidney stones, excessive urination, abdominal pain, fatigue, and depression. These symptoms are related to the imbalance of calcium in the body due to overactive parathyroid glands.
What factors can contribute to the development of hyperparathyroidism?
Factors that can lead to hyperparathyroidism vary, but they usually include benign growths on the parathyroid glands, hereditary conditions, or radiation treatment of the neck. These factors cause an increase in parathyroid hormone (PTH) release, impacting calcium regulation.
What distinguishes primary from secondary hyperparathyroidism?
Primary hyperparathyroidism occurs when one or more of the parathyroid glands are overactive, causing high calcium levels. In contrast, secondary hyperparathyroidism is a reaction to low calcium levels in the blood, often due to chronic kidney disease, where the body tries to correct the imbalance by overproducing PTH.
How does an elevated calcium level relate to hyperparathyroidism?
Elevated calcium levels are often a hallmark of hyperparathyroidism, as the condition leads to the overproduction of PTH, which in turn increases calcium release from the bones into the bloodstream.
What are the potential complications associated with untreated hyperparathyroidism?
If untreated, hyperparathyroidism can lead to complications such as osteoporosis, kidney stones, cardiovascular issues, and nervous system problems. Early detection and treatment can help mitigate these risks.
What dietary restrictions are recommended for individuals with hyperparathyroidism?
Individuals with hyperparathyroidism are typically advised to maintain adequate hydration and limit foods high in calcium and phosphorus. They may also be guided to avoid supplemental calcium and to consult with healthcare providers for personalized dietary recommendations.

