Peripheral neuropathy affects the body’s peripheral nerves, which are responsible for sending signals between the brain, spinal cord, and the rest of the body. The condition can cause pain, weakness, and numbness, primarily in the hands and feet. Patients and their loved ones frequently have concerns about how peripheral neuropathy may impact life expectancy. The relationship between peripheral neuropathy and life span can vary widely depending on the underlying cause of the neuropathy, its severity, and how well it is managed.
If peripheral neuropathy results from a manageable condition such as diabetes, controlling blood sugar levels can play a significant role in prognosis. With appropriate management, individuals with diabetic neuropathy can have a normal life expectancy. However, when peripheral neuropathy is caused by more severe or progressive conditions, like certain types of cancers or genetic diseases, it can potentially have a more direct impact on life expectancy.
Management strategies for peripheral neuropathy often revolve around treating the underlying condition and alleviating symptoms. There is a spectrum of treatments available that can improve quality of life and, in some cases, slow the progression of the disease. Supportive care, medications, physical therapy, and lifestyle modifications contribute to managing peripheral neuropathy. Therefore, prognosis for patients with neuropathy relies heavily on the nature and treatment of its root cause, as well as the overall health and lifestyle choices of the individual.

I am a Nurse Practitioner licensed across multiple states, with experience in cardiology, nephrology, and family medicine. My current focus is on primary care, where I advocate for a holistic approach to healthcare, often recommending functional medicine to patients when suitable.
Overview of Peripheral Neuropathy
Peripheral neuropathy encompasses a range of disorders where the peripheral nerves are damaged, which can significantly impact quality of life and overall health.
Definition and Pathophysiology
Peripheral neuropathy is the result of damage to the peripheral nerves, the extensive communication network that transmits information between the central nervous system (the brain and spinal cord) and every other part of the body. These nerve damages can disrupt nerve signal transmission and damage the nerve fibers, leading to various symptoms, which can range from pain and numbness to weakness, depending on the type of nerves affected.
Types and Causes
Sensory nerves, motor nerves, and autonomic nerves can all be affected by neuropathy, leading to their respective symptoms and complications. There are various causes of peripheral neuropathy, including:
- Diabetes: the most common cause leading to neuropathy
- Infections: such as shingles or HIV
- Vitamin deficiencies: particularly B vitamins
- Toxins: exposure to heavy metals or chemicals
- Genetics: inherited forms of neuropathy
- Autoimmune diseases: like rheumatoid arthritis and lupus
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
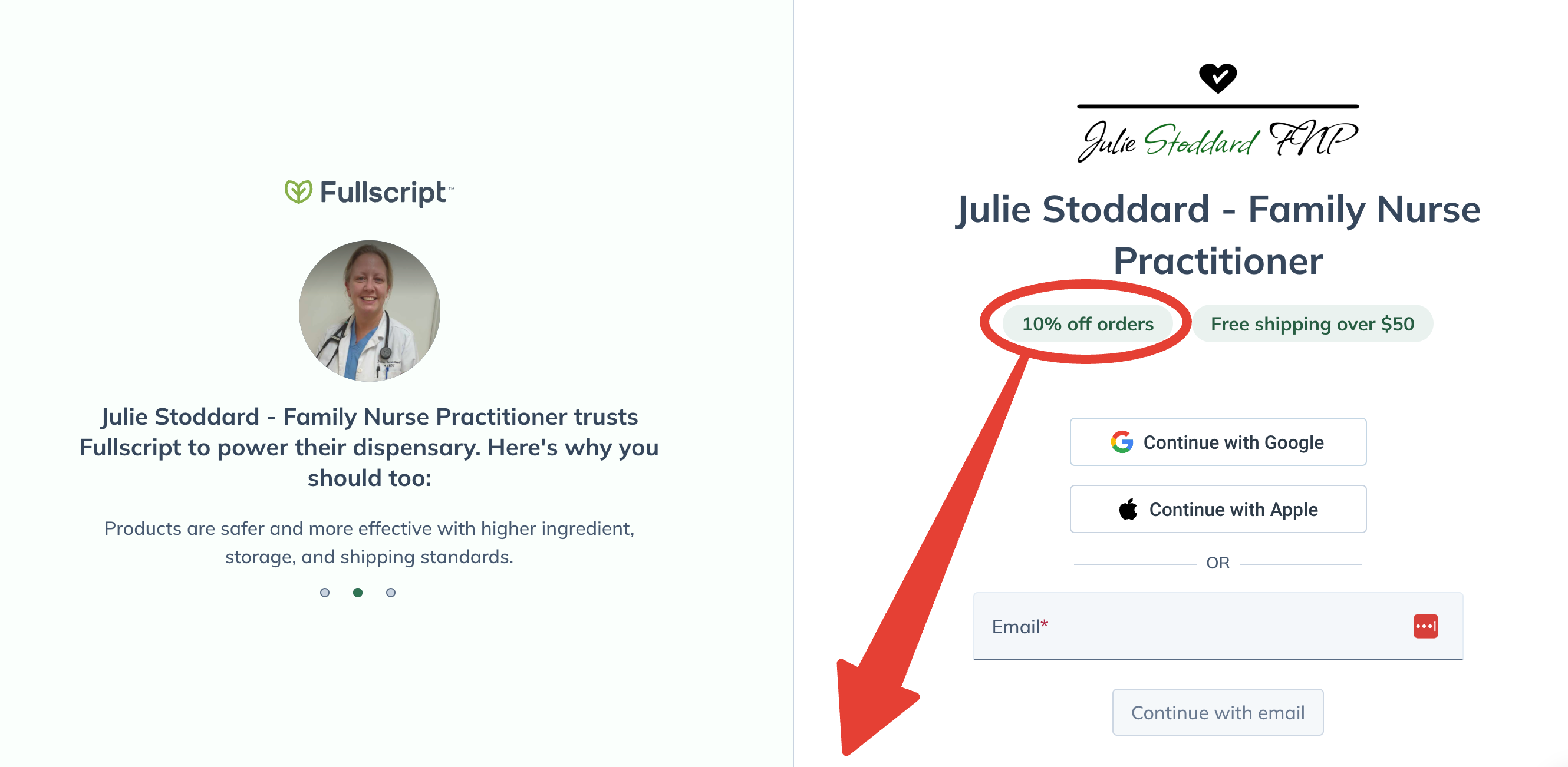
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
Influencing Factors on Life Expectancy
Life expectancy with peripheral neuropathy can vary, influenced by several factors including the severity of the condition, the presence of other health issues, demographic attributes, and lifestyle choices.
Severity and Progression of Neuropathy
The severity of peripheral neuropathy and the rate at which it progresses play vital roles in impacting life expectancy. Patients with mild symptoms might experience minimal impact on their daily lives, whereas severe and rapidly progressing neuropathy can lead to complications that may decrease life expectancy.
Underlying Health Conditions
Comorbid health conditions, especially those that are the root cause of neuropathy, significantly affect life expectancy. For instance, neuropathy due to diabetes may have different implications compared to neuropathy stemming from autoimmune diseases.
Age and Gender
Demographic factors such as age and gender also influence the prognosis of peripheral neuropathy. Typically, younger patients may fare better due to a greater capacity for nerve regeneration, whereas data suggests there may be gender differences in the experience and management of neuropathic symptoms.
Lifestyle and Management
How individuals manage their neuropathy through lifestyle choices and treatment adherence is key. Those who engage in regular exercise, maintain a balanced diet, and follow their treatment regimens consistently can have a better quality of life and potentially improved life expectancy.
Prognosis and Survival Rates
Peripheral neuropathy encompasses a range of disorders that have varying prognoses and survival rates based on their underlying causes. The impact on life expectancy often relates to the conditions associated with neuropathy and their management.
Statistics and Research Findings
Research indicates that the prevalence of peripheral neuropathy increases with age. Certain types of neuropathy, such as diabetic neuropathy, are observed in nearly half of individuals with long-standing diabetes. Diseases like leprosy continue to be significant causes of neuropathy globally, especially in South Asia. However, no single medication has emerged as a clear winner in effectively treating neuropathy symptoms across the board, which underscores the complexity of managing the condition.
Role of Early Detection and Treatment
Early detection and appropriate treatment of peripheral neuropathy can mitigate symptoms and, in some cases, slow the progression of the disease. Diagnoses like those related to paclitaxel-induced acute pain suggest potential benefits from timely interventions like topical cryotherapy. Effective management of symptoms and underlying conditions plays a crucial role in maintaining quality of life and may influence survival rates in individuals with neuropathy-induced complications.
Complications and Risks
Peripheral neuropathy can lead to significant health complications and risks, affecting patients’ overall well-being and daily function.
Associated Complications
Peripheral neuropathy can lead to a range of associated complications that may reduce life expectancy if not managed properly. These include:
- Infections and Ulcers: Loss of sensation may prevent early detection of cuts and injuries, particularly in the feet, leading to infections or ulcers.
- Falls and Injuries: Decreased muscle strength and loss of sensation can result in falls, leading to injuries such as fractures.
Impact on Daily Living and Quality of Life
The impact on daily living and quality of life for individuals with peripheral neuropathy can be profound, including:
- Physical Limitations: Chronic pain and muscle weakness can restrict mobility and the ability to perform daily tasks.
- Mental Health: The ongoing discomfort and disability can cause psychological distress, such as depression and anxiety, affecting life quality.
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
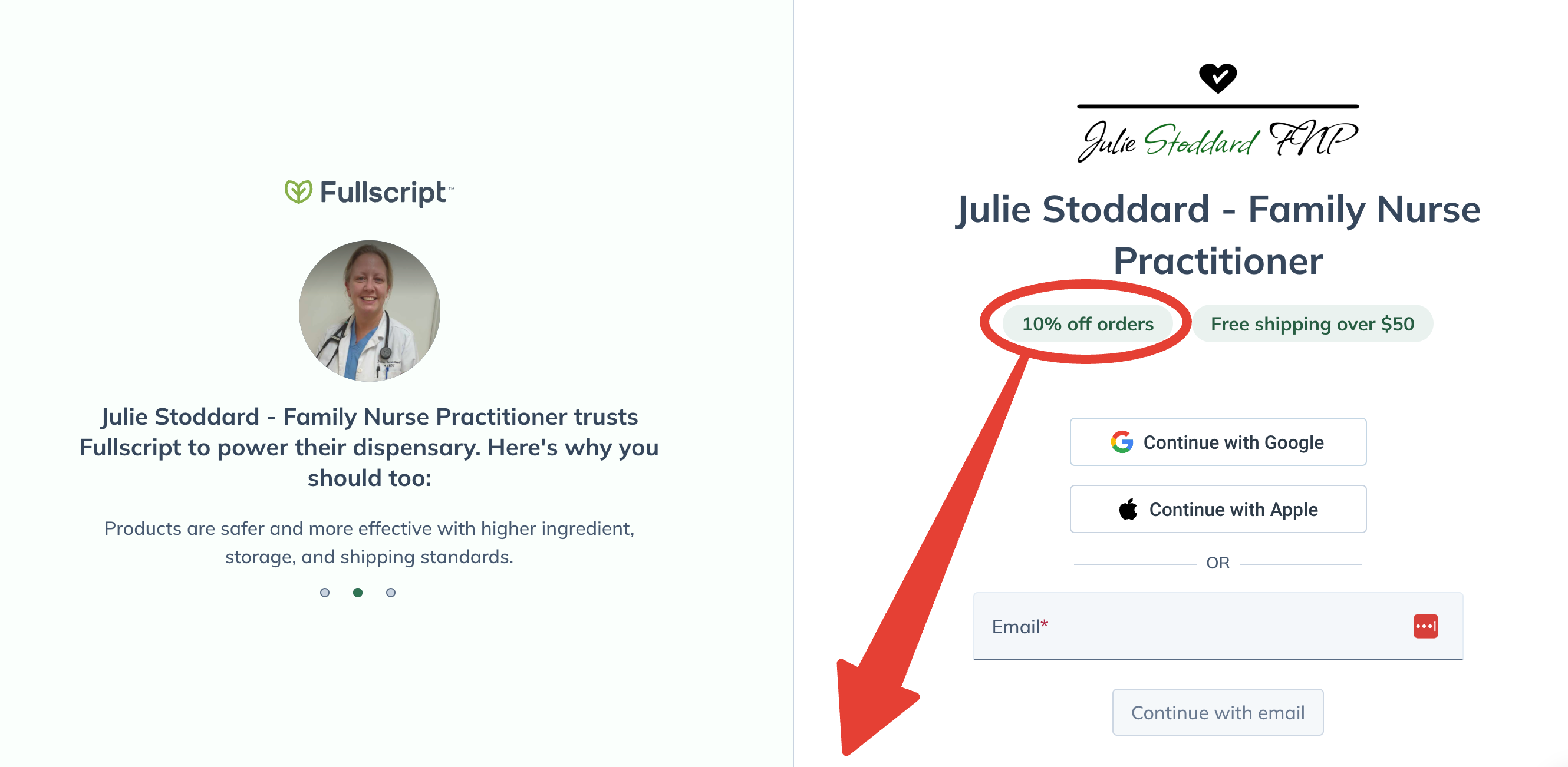
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
Therapeutic Interventions
Therapeutic interventions for peripheral neuropathy focus on managing symptoms and slowing disease progression. Treatment strategies may include medications, physical therapy, and, in certain cases, surgical options.
Medications
Medications are a cornerstone in the management of peripheral neuropathy symptoms. Pain relievers like over-the-counter pain medications may be used for mild symptoms, while prescription-strength drugs could be necessary for more severe pain. These may include antidepressants which alter pain perception, or anticonvulsants that stabilize nerve cells. According to Harvard Health, no one medication stands out as the most effective, underscoring the need for individualized treatment plans.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation play important roles in improving mobility and function. Exercises tailored for neuropathy patients can help maintain muscle strength and reduce discomfort. Balance training is essential to minimize the risk of falls due to sensory loss. The Mayo Clinic Research highlights interventions like cryotherapy that could relieve pain from peripheral neuropathy, demonstrating the potential benefits of complementary therapies.
Surgical Options
Surgical interventions are considered when neuropathy is caused by nerve compression or when other treatments fail to relieve symptoms. The procedures aim to relieve pressure on the affected nerves and to repair nerve damage whenever possible. These might include decompressive surgeries or surgical repair of nerve injuries. The determination to proceed with surgical intervention takes into account the underlying cause and the individual’s overall health status.
Lifestyle Modifications and Support
Effective management of peripheral neuropathy often involves lifestyle modifications that can help to control symptoms and improve overall quality of life. By addressing factors such as diet, physical activity, and psychological support, individuals may find relief and lead more comfortable lives.
Dietary Changes
Diet plays a crucial role in managing peripheral neuropathy. A diet rich in B vitamins, especially B12 and folate, can support nerve health. Foods like lean meats, eggs, and dairy products are beneficial. For plant-based options, individuals can turn to fortified cereals and nutritional yeasts. It’s also recommended to include antioxidant-rich foods such as berries, nuts, and leafy greens to combat oxidative stress, which can contribute to nerve damage.
Exercise and Physical Activity
Regular physical activity is essential for individuals with peripheral neuropathy. Exercise can improve muscle strength, decrease neuropathic pain, and enhance coordination. It’s important to start slowly with low-impact activities like swimming or cycling. A structured exercise program should aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week, coupled with strength training exercises at least two days a week.
Psychosocial Support
Dealing with peripheral neuropathy can be challenging not just physically, but emotionally as well. Support groups or counseling can be instrumental in managing the psychological aspects of chronic illness. They can provide a platform for sharing experiences and coping strategies. Access to psychosocial support can lead to better management of the condition and improved mental health.
Innovations in Treatment
Advancements in the treatment of peripheral neuropathy offer new hope to patients, as recent developments aim to improve life expectancy and quality of life. Cutting-edge therapies and technological innovations are at the forefront of these advancements.
Emerging Therapies
Clinical trials have shown that new pharmacological agents like BP4L-18:1:1 are promising in the treatment of neuropathic pain, a common consequence of peripheral neuropathy. These novel medications offer potential alternatives to traditional pain management and focus on the underlying nerve damage.
Technological Advancements
Medical devices are also transforming the management of peripheral neuropathy. Studies at UAMS have highlighted breakthrough treatment methods such as neuromodulation which can significantly alleviate pain associated with diabetic neuropathy. These advancements demonstrate the effective integration of technology and medicine in extending both the longevity and the quality of life for those affected by this condition.
Clinical Trials and Research
Clinical trials and research are crucial for advancing the understanding and treatment options for peripheral neuropathy. They play a vital role in improving life expectancy and quality of life for patients.
Ongoing Studies
The Mayo Clinic is a frontrunner in conducting clinical trials on peripheral neuropathy, exploring various treatments to alleviate symptoms like pain, numbness, and muscle weakness. They are examining the effects of topical cryotherapy on pain relief for those affected by neuropathy due to chemotherapy.
Future Outlook
Research institutions like Harvard Health and Weill Cornell Medicine are tirelessly working towards finding the best medications and treatments. Studies on medications such as nortriptyline have yielded promising results in improving discomfort in patients. Preclinical tests on non-opioid molecules show potential in treating chronic neuropathic pain, hinting at future advances in non-opioid pain management.
Clinical trials underscore the ongoing commitment to enhancing life expectancy and patient outcomes, indicating a hopeful future for individuals with peripheral neuropathy.
Patient Resources and Support Networks
Patients with peripheral neuropathy can access a variety of resources and support networks tailored to provide assistance and information. These avenues offer valuable guidance and community support, enhancing quality of life and empowering patients with knowledge about their condition.
Support Groups and Communities
Support groups and communities provide a platform for individuals to share their experiences and gain emotional support from others facing similar challenges. For example, the Foundation for Peripheral Neuropathy offers a comprehensive directory of support groups organized by geographical locations. Similarly, online forums such as the Neuropathy Association’s online community also provide a virtual space for discussion and connection.
Educational Materials and Resources
Educational materials and resources equip patients with up-to-date information about peripheral neuropathy, treatments, and research advances. The Harvard Health publications provide readers with insights into newer perspectives on the condition. Additionally, the Mayo Clinic’s Peripheral Neuropathy Clinical Trials page details ongoing research that could potentially lead to new treatments, giving patients an outlook on the future of neuropathy management.
Legal and Social Considerations
Peripheral neuropathy can significantly affect an individual’s daily life, leading to a need for comprehensive legal and social considerations that address the challenges faced by those with the condition.
Disability Rights and Accommodations
Under the Americans with Disabilities Act (ADA), individuals with peripheral neuropathy may be entitled to reasonable accommodations to help them carry out essential life activities. This could include access to assistive technologies, modifications in the workplace, and other necessary adjustments that acknowledge the limitations imposed by their condition.
Employment and Financial Aspects
The financial impact of living with peripheral neuropathy is considerable. Those affected may encounter difficulties maintaining employment due to physical limitations. They might be eligible for disability benefits through programs like Social Security Disability Insurance (SSDI). Employers are required to consider job restructuring and part-time or modified work schedules to accommodate an employee’s condition if it qualifies under the ADA.
Frequently Asked Questions
Peripheral neuropathy raises many concerns, particularly regarding its impact on lifespan and daily living. The following frequently asked questions address the most pressing concerns related to the condition’s progression and management.
What is the impact of peripheral neuropathy on life expectancy?
Peripheral neuropathy itself does not typically reduce life expectancy, but it can be a complication of several serious conditions that might. The impact on lifespan largely depends on the underlying cause of the neuropathy.
Is it possible to manage symptoms and have a quality life with peripheral neuropathy?
Yes, with appropriate treatment and lifestyle adjustments, many people with peripheral neuropathy lead fulfilling lives. Pain management, physical therapy, and, in some cases, medications can significantly alleviate symptoms.
Can the progression of neuropathy be halted or reversed?
In some cases, the progression of neuropathy can be halted or even reversed, especially if it’s caused by a treatable condition. Proper management of underlying conditions, such as diabetes, can stabilize or improve the symptoms.
What factors influence the progression rate of peripheral neuropathy?
The progression rate of peripheral neuropathy is influenced by factors such as the type of neuropathy, the severity and control of the underlying cause, and the individual’s overall health and lifestyle choices.
How does neuropathy in feet affect the overall health and lifespan?
Neuropathy in the feet can lead to balance issues and falls, increases the risk for foot injuries and infections, and may contribute to a sedentary lifestyle, which can negatively influence overall health and potentially impact lifespan.
What are the potential complications of severe peripheral neuropathy?
Severe peripheral neuropathy can lead to a number of complications including severe pain, infections, foot ulcers, falls, and, in extreme cases, may require amputation. These complications can significantly affect an individual’s health and quality of life.

