Young-onset dementia is a term that encompasses various forms of dementia diagnosed in individuals under the age of 65. One such form is young-onset frontotemporal dementia, which represents a group of brain disorders caused by the progressive loss of nerve cells in the frontal and/or temporal lobes. These regions are primary for controlling judgment, social behavior, emotions, speech, and language. While less common than Alzheimer’s disease in the younger population, frontotemporal dementia (FTD) presents distinct challenges due to its early onset and the unique symptoms it entails.
FTD often leads to significant changes in personality and behavior, which can be misinterpreted as psychiatric problems rather than neurological. In particular, behavioral variant frontotemporal dementia is marked by inappropriate actions, lack of empathy, and difficulty in managing routine tasks. Language variants of FTD can severely disrupt a person’s ability to communicate. These symptoms not only disrupt the patient’s life but also have a profound impact on their families and caregivers.
Recognizing the signs and risk factors of young-onset FTD is critical. A study published in JAMA Neurology in December 2023 has elucidated several factors associated with a higher risk for developing young-onset dementia. Timely diagnosis and intervention can lead to better management, helping individuals maintain their independence and quality of life for as long as possible.

I am a Nurse Practitioner licensed across multiple states, with experience in cardiology, nephrology, and family medicine. My current focus is on primary care, where I advocate for a holistic approach to healthcare, often recommending functional medicine to patients when suitable.
Understanding Frontotemporal Dementia (FTD)
Frontotemporal dementia (FTD) represents a cluster of brain disorders known for their impact on personality, behavior, and language. It stands distinct from other types of dementia with its unique symptoms and demographic.
Defining Frontotemporal Dementia
Frontotemporal dementia, also known as frontotemporal lobar degeneration, refers to a spectrum of disorders caused by progressive nerve cell loss in the frontal and temporal lobes of the brain. Key areas affected include those responsible for decision-making, behavioral control, emotion regulation, and language skills. The term “FTD” is an umbrella designation, under which several subtypes fall, each with varying manifestations. Some patients may exhibit profound behavioral changes, known as behavioral variant FTD (bvFTD), while others may experience language-related symptoms, known as primary progressive aphasia (PPA).
Epidemiology of FTD
Epidemiological data on frontotemporal dementia reveal that it most commonly emerges at a younger age than other forms of dementia, such as Alzheimer’s disease. It typically affects individuals between the ages of 45 and 65. However, cases have been diagnosed both earlier and later in life. While FTD is less prevalent than Alzheimer’s disease, it is a significant cause of dementia in younger populations. Studies suggest genetics play a role in many instances, with family history contributing to the likelihood of developing the condition.
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
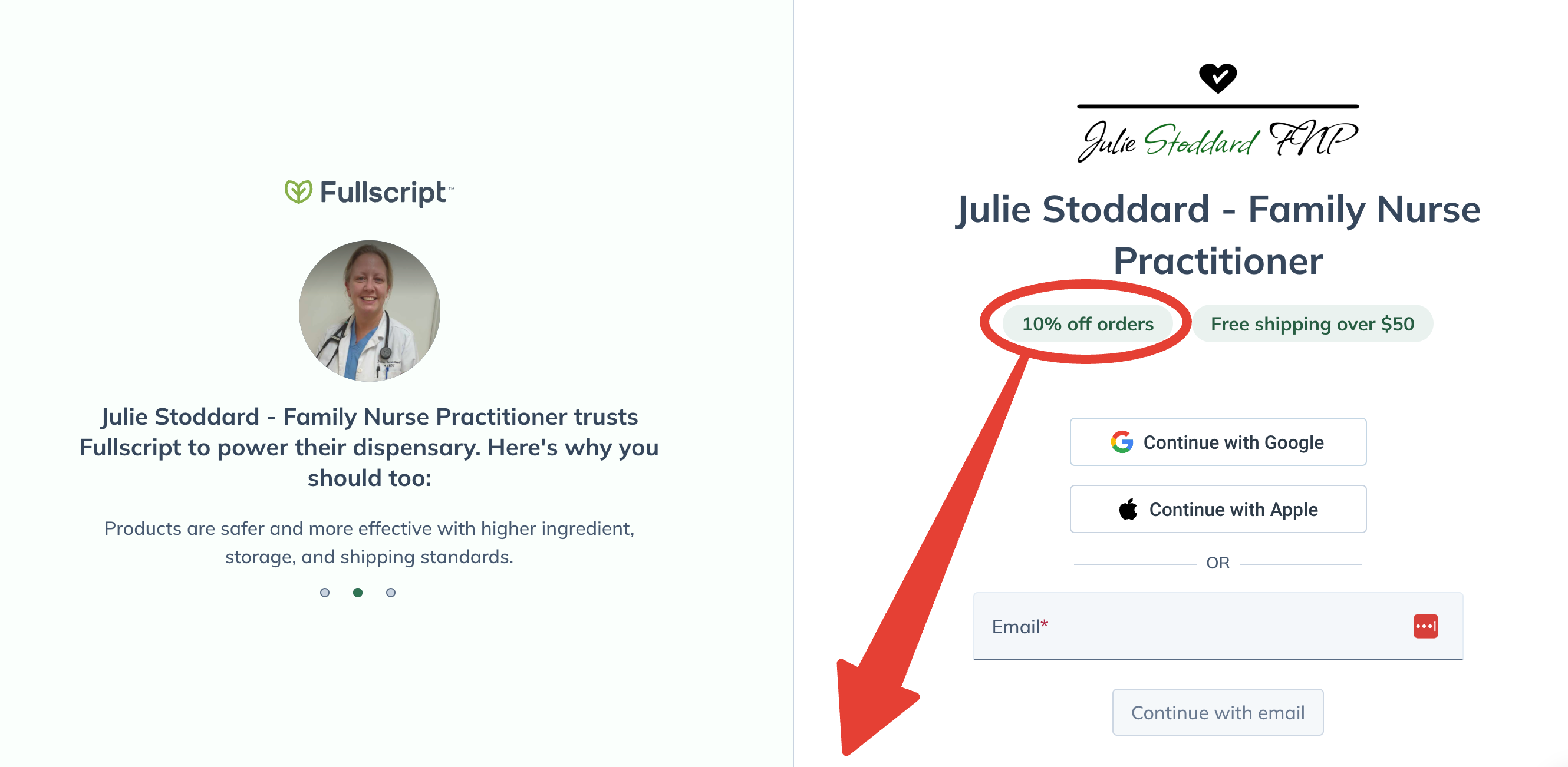
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
Symptoms and Clinical Phenotypes
Frontotemporal dementia (FTD) manifests in distinct syndromes affecting behavior, language, and motor functions. Identifying clinical phenotypes is important for diagnosis and management, as symptoms can vary widely among individuals.
Behavioral and Emotional Changes
Individuals with FTD may undergo significant personality changes. They exhibit behavioral and emotional shifts, such as apathy, that are stark departures from their prior character. Family members often notice these changes as one of the first signs of the disease. Examples include social withdrawal, loss of inhibitions, or a diminished ability to empathize with others.
Language and Communication Impairment
Language and communication issues are hallmarks of certain FTD phenotypes. Some might struggle with word retrieval or sentence construction, a condition known as Primary Progressive Aphasia. Depending on the affected brain regions, patients may also exhibit poor speech production or comprehension, reflecting a degeneration in the brain’s language centers.
Movement Disorders and Motor Symptoms
Motor symptoms in FTD can manifest as movement disorders, including poor coordination, muscle spasms, or Parkinsonism, which is characterized by tremors and rigidity. Individuals might exhibit clumsiness or difficulty with fine motor skills, signaling the involvement of motor neurons. These symptoms are a clinical phenotype known as FTD with motor neuron disease.
Etiology and Risk Factors
Frontotemporal dementia (FTD) is a complex condition, where both genetics and protein misfolding play pivotal roles as etiological factors. Understanding these elements can illuminate potential risk factors and the development of the disease.
Genetic Factors and Family History
A significant proportion of FTD cases have a genetic component. Mutations in several genes, such as C9orf72, MAPT, and GRN, strongly influence the heritability of the disorder. Family history is a key risk factor; individuals with a family history of FTD or dementia are at an increased risk of developing FTD themselves. In families with a known genetic mutation, the risk of passing the same mutation to offspring is typically 50%.
Protein Misfolding and Tau Pathology
Protein misfolding, particularly involving the tau protein, is a hallmark of certain types of FTD. Pathological tau accumulations lead to neurodegeneration. The presence of tau pathology is indicative of the cell-to-cell spread of misfolded proteins, which correlates with disease progression. Although not all variants of FTD are associated with tau proteinopathy, when it is present, it significantly increases the severity and progression of disease symptoms.
Understanding these genetic and pathological factors is important for identifying individuals at risk and for the development of targeted therapies.
Brands Fullscript carries include but are not limited to:
- Life Entensions
- Thorne
- Pure Encapsulations
- Metagenics
- Designs for Health
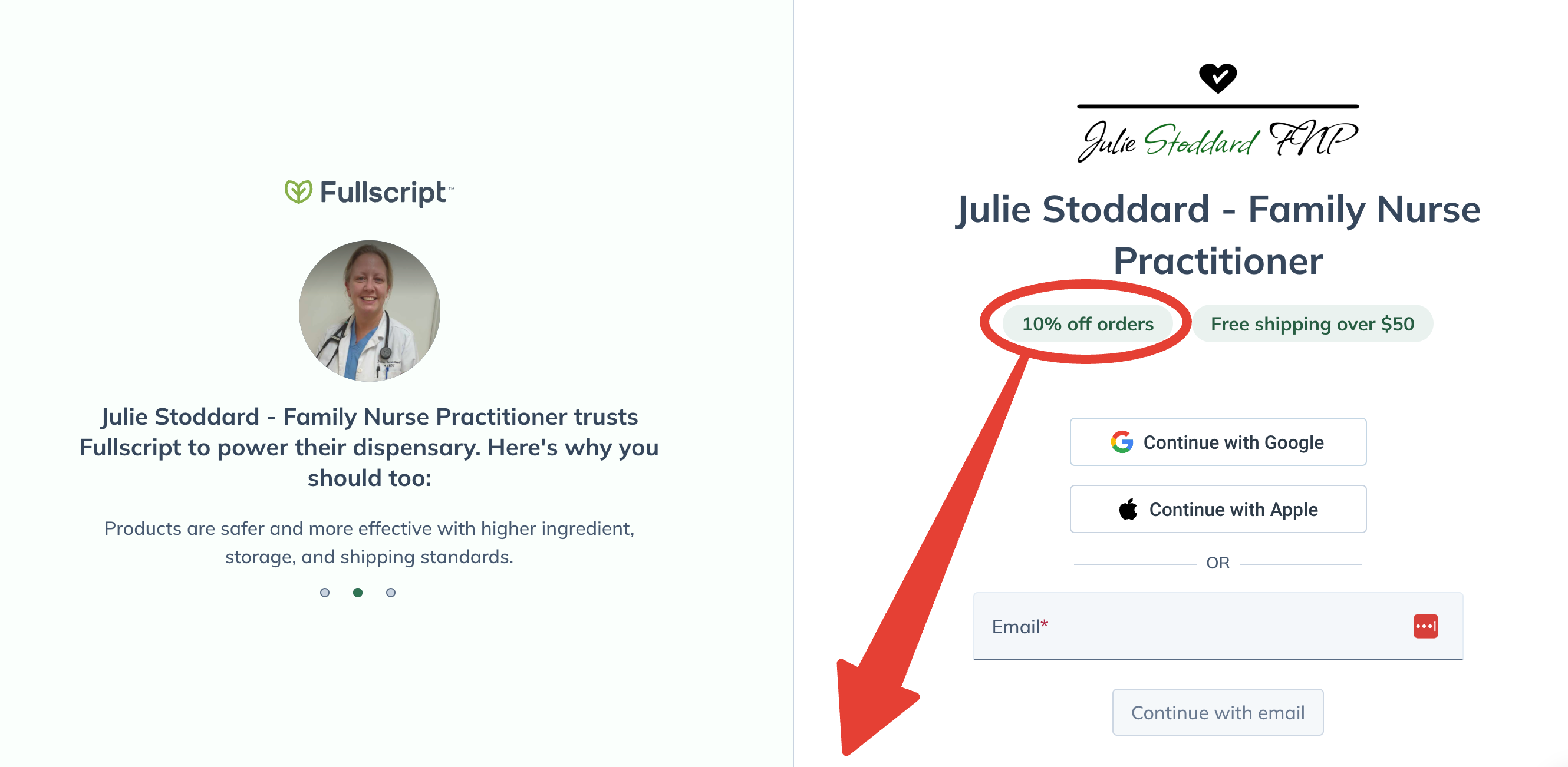
Lifetime 10% Off All Products
Enjoy access to FullScript™ through my practitioner link, where 2000+ premium supplement products await!
No purchase required today.
Free shipping on all orders over $50.
Diagnosis and Medical Imaging
Diagnosis of young onset frontotemporal dementia is multifaceted, requiring a combination of advanced medical imaging techniques and comprehensive cognitive assessments. This integrated approach helps in identifying characteristic brain changes and assessing the cognitive and behavioral functions, which are needed for an accurate diagnosis.
Neuroimaging Techniques
Magnetic Resonance Imaging (MRI) is a cornerstone in the diagnosis of frontotemporal dementia, as it can reveal atrophy in the frontal and temporal lobes of the brain. Details such as the extent of atrophy and the specific regions affected are vital clues that assist clinicians in distinguishing frontotemporal dementia from other forms of dementia.
- Computed Tomography (CT): Although less sensitive than MRI, it is sometimes used when MRI is not available or if the patient has contraindications to MRI screening.
- Positron Emission Tomography (PET): This imaging technique, including both Amyloid PET and Tau PET, helps to visualize metabolic activity and the deposition of abnormal proteins in the brain, which further supports the distinction between frontotemporal dementia and other neurodegenerative diseases.
Cognitive and Neuropsychiatric Assessment
The Mini-Mental State Examination (MMSE) is a brief 30-point questionnaire often used to screen for cognitive impairment. However, additional tests are usually necessary to discern the nuances of frontotemporal dementia, since the MMSE may not always detect it.
- Neuropsychiatric Evaluation: This involves a thorough assessment of behavior, personality, and language, which can be significantly impacted in frontotemporal dementia. It helps to identify specific symptoms such as apathy, impulsivity, or language difficulties.
Genetic Testing: While not a standard part of the initial diagnostic process, genetic testing can be important in cases with a family history suggestive of a genetic component to the disease. Identifying mutations can confirm the diagnosis and assist with family planning.
Clinical Subtypes of FTD
Frontotemporal Dementia (FTD) is categorized into several clinical subtypes. Each subtype has distinctive symptoms and characteristics, impacting language, behavior, and motor functions differently.
Behavioral Variant FTD (bvFTD)
Behavioral Variant Frontotemporal Dementia, commonly referred to as bvFTD, is characterized by significant changes in personality, empathy, and conduct. Patients often exhibit socially inappropriate behavior, emotional blunting, and a lack of insight into their condition. This subtype may also impact language or thinking skills, although these are not the primary domains affected.
Primary Progressive Aphasia (PPA)
Primary Progressive Aphasia predominantly affects language capabilities. This subtype is further divided into two main categories: semantic dementia and progressive non-fluent aphasia. In semantic dementia, an individual’s understanding of words and objects deteriorates, while progressive non-fluent aphasia involves a breakdown in the production of speech, making it laborious and halting.
Frontotemporal Dementia with Motor Neuron Disease
This subtype of FTD includes a combination of cognitive symptoms associated with bvFTD or PPA and motor symptoms reminiscent of amyotrophic lateral sclerosis (ALS), also known as motor neurone disease. Patients may experience muscle weakness, twitching, and loss of coordination. Some may also develop parkinsonism—a syndrome characterized by tremors, stiffness, and bradykinesia (slow movement).
Management and Treatment Strategies
Effective management of young onset frontotemporal dementia (FTD) hinges on accurately identifying the symptoms and implementing tailored therapeutic approaches. Equally important is the provision of robust support for patients and caregivers to alleviate stress and improve quality of life.
Therapeutic Approaches
For FTD, there is currently no cure, but a range of treatments can help manage the symptoms. Healthcare providers may prescribe antidepressants to address behavioral symptoms or recommend therapy to mitigate language difficulties. Clinical trials continue to explore innovative treatments, focusing on altering the disease’s pathology. Though not definitive cures, these interventions aim to slow disease progression and provide symptom relief.
- Medication: Antidepressants can help control behavioral changes.
- Therapy: Speech and occupational therapies can assist with language and daily tasks.
Support for Patients and Caregivers
Caring for someone with FTD often places considerable stress on caregivers, emphasizing the necessity of dedicated support networks. Healthcare providers should direct caregivers to resources that offer emotional and practical assistance.
- Support Groups: They provide a platform for sharing experiences and coping strategies.
- Caregiver Training: Educates on managing symptoms of FTD and enhancing patient care.
Therapeutic approaches and caregiver support are integral in the management of FTD, ensuring patients receive comprehensive care tailored to their specific needs.
Research and Future Directions
Frontotemporal dementia (FTD) research is rapidly advancing, with genetic discoveries and the development of potential drug targets showing promise for future treatments of this form of neurodegeneration. This section explores recent significant findings and the next steps in research.
Genetic Research and Biomarkers
Researchers have linked numerous genetic mutations to frontotemporal dementia, signifying a key role genetics plays in FTD. Alongside these genetic associations, scientists aim to identify biomarkers that can reliably indicate the presence of FTD and track its progression. One study, for instance, investigates the crosstalk between peripheral immune cells and dysfunctional microglia and its effects on neurodegeneration, which could lead to valuable prognostic and diagnostic tools.
- Notable Genes: C9orf72, GRN, MAPT
- Biomarkers of Interest: tau proteins, neurofilaments
Potential Targets for Drug Development
The discovery of proteins involved in frontotemporal dementia opens new avenues for potential therapies. Proteins such as tau and those related to FUS pathology are implicated in the disease’s pathology. Some proteins found in the brain are linked directly to FTD, providing a target for research into pharmacological interventions. Furthermore, gliosis, the proliferation of glial cells in response to injury, has also been observed in FTD patients, which might serve as another therapeutic target. Clinical trials are underway to explore these targets, with the goal of slowing or stopping the neurodegenerative process.
- Proteins Involved: tau, FUS
- Pathologies Observed: gliosis, nerve cell damage
Living with FTD
Living with Frontotemporal Dementia (FTD) involves adapting daily life and preparing for the future through legal and financial planning. Individuals and their families often face challenges including personality changes and loss of empathy, which necessitate significant lifestyle adjustments.
Daily Life Adjustments
Individuals affected by frontotemporal dementia (FTD) often encounter inflexibility in their daily routines and psychiatric symptoms, underscoring the importance of adjusting to everyday life. Impairments in executive function frequently result in challenges with planning and executing tasks, while compulsive behaviors necessitate the establishment of structured schedules.
- Routine establishment: A consistent daily schedule helps reduce confusion and anxiety.
- Home safety modifications: Removing hazards can prevent accidents, considering that individuals may lack judgment or awareness of potential dangers.
Social interactions are also affected as they may display a loss of empathy. Families and caregivers can facilitate communication by setting clear rules and guidelines for encounters both in and outside the home.
Legal and Financial Planning
FTD can also cause changes in a person’s ability to manage finances, making early legal and financial planning paramount.
- Power of Attorney: Assigning a trusted person to make decisions helps protect the individual’s interests when they cannot do so themselves.
- Living Trusts: Ensuring assets are managed according to the person’s wishes can provide security for their care.
It is also vital to consider potential health complications such as infections or thyroid disease associated with FTD’s neuropathological changes. Crafting a care plan with healthcare professionals can address not only current symptoms but also future health considerations.

